Drinking a glass of grapefruit juice in the morning might seem like a healthy habit-until it turns dangerous. For people taking certain medications, that refreshing citrus drink can trigger serious, even life-threatening reactions. It’s not about allergies or sugar. It’s about how grapefruit juice quietly shuts down your body’s ability to process drugs safely. This isn’t a myth or a warning you can ignore. It’s a well-documented, clinically proven interaction that affects more than 85 prescription medications. And if you’re on one of them, even one glass can change how your body handles your medicine-sometimes permanently.
How Grapefruit Juice Changes Your Medication
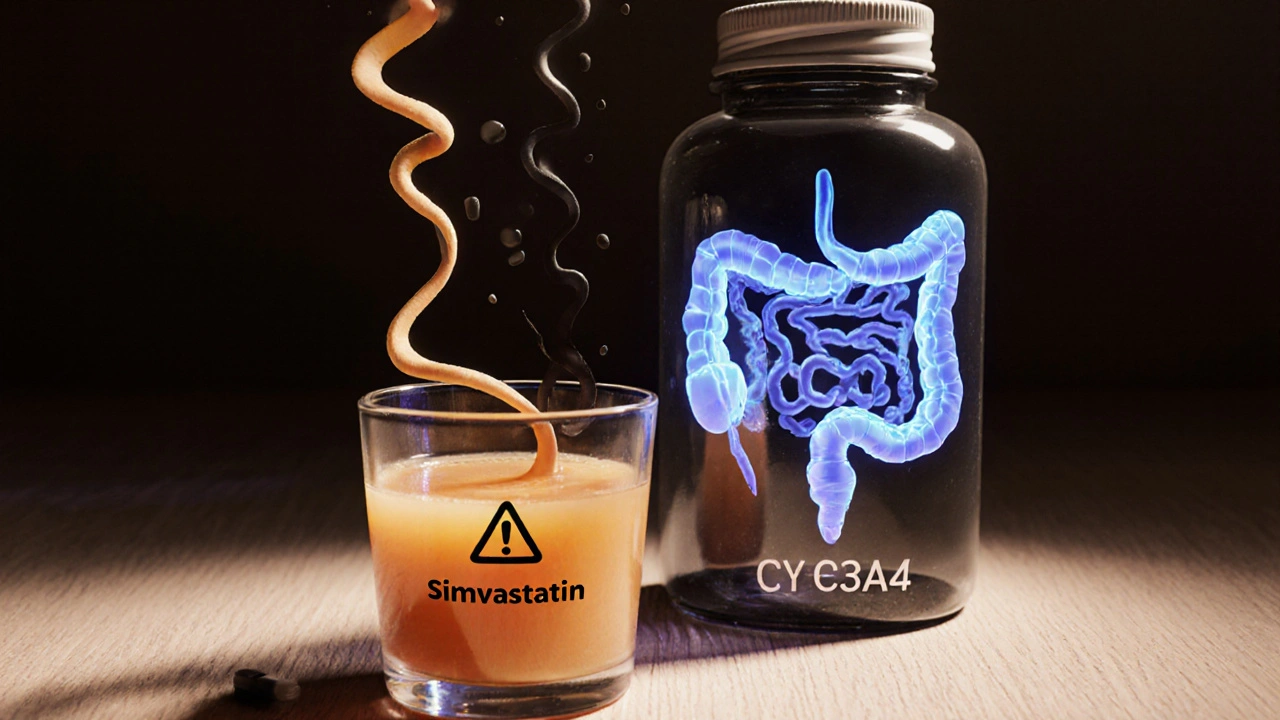
Grapefruit juice doesn’t just mix poorly with some drugs-it actively rewires how your body absorbs them. The culprit? Furanocoumarins, natural chemicals found in grapefruit, especially in the peel and pulp. These compounds attack an enzyme in your gut called CYP3A4. This enzyme normally breaks down about half of all oral medications before they enter your bloodstream. When grapefruit juice blocks it, your body absorbs way more of the drug than it should.
What happens next is simple: too much drug in your blood. That means stronger effects-and higher risk of side effects. For some medications, that’s the difference between feeling better and ending up in the hospital. The worst part? The effect lasts a long time. One 6.7-ounce glass can block CYP3A4 for up to 72 hours. That means even if you take your pill at night and drink juice in the morning, you’re still at risk.
Unlike other food-drug interactions that require timing precision, grapefruit juice doesn’t care when you take it. If you’re on a medication that interacts with it, you need to avoid it completely while you’re taking the drug. There’s no safe window. No "just once" exception. And no way to predict how your body will react.
Medications That Can Become Dangerous with Grapefruit
Not all drugs are affected equally. But some of the most commonly prescribed medications fall into the high-risk category. Here are the big ones:
- Statins (cholesterol drugs): Simvastatin (Zocor) is the most dangerous. Just one glass of grapefruit juice daily for three days can triple your blood levels of this drug. That raises your risk of rhabdomyolysis-a condition where muscle tissue breaks down and can lead to kidney failure. Atorvastatin (Lipitor) is less risky, but still affected. Pravastatin and rosuvastatin? Safe. No interaction.
- Calcium channel blockers (blood pressure meds): Felodipine (Plendil) sees a 5-fold increase in blood levels. Nifedipine (Procardia) jumps 3.3 times. Amlodipine (Norvasc)? Minimal effect. If you’re on blood pressure meds, check which one you’re taking.
- Immunosuppressants: Cyclosporine (Neoral), used after organ transplants, can spike 50-60% in concentration. That raises the risk of kidney damage. Tacrolimus has less interaction, making it a safer alternative for some patients.
- Antiarrhythmics: Amiodarone (Cordarone) can increase by 30-40%, raising the chance of irregular heart rhythms.
- Other high-risk drugs: Some sedatives like triazolam, certain antidepressants, and even some cancer drugs like docetaxel can become toxic when mixed with grapefruit.
On the flip side, many common drugs show no interaction. Trazodone (for sleep or depression), zolpidem (Ambien), and most antibiotics are safe. But unless your doctor or pharmacist confirms it, assume the worst.
Why Some People Are More at Risk
Not everyone reacts the same way. One study showed that after drinking grapefruit juice, some people had zero increase in drug levels-while others saw an 8-fold jump. Why? Because CYP3A4 enzyme levels vary naturally between individuals. People with higher baseline levels in their gut get hit harder. But here’s the problem: no test can measure this before you start a drug. You can’t know your risk until something goes wrong.
Age also matters. People over 65 are especially vulnerable. They’re more likely to be on multiple medications and more likely to drink grapefruit juice regularly. According to USDA data, older adults make up 40% of grapefruit consumers. On average, they take 3-5 prescription drugs. That’s a dangerous combo.
Even the type of grapefruit matters. White grapefruit has more furanocoumarins than red. Fresh-squeezed juice is stronger than store-bought or pasteurized. And don’t assume "no sugar added" means safer-it’s still the same chemicals causing the problem.

What About Other Citrus Fruits?
Not all citrus is the same. Seville oranges (used in marmalade) and pomelos contain the same furanocoumarins as grapefruit. So if you’re avoiding grapefruit, avoid these too. Sweet oranges (like navel or Valencia) and lemons? Safe. They don’t contain the harmful compounds. Limes? Mostly safe, though some varieties may have trace amounts. Stick to sweet orange juice if you want citrus with your meds.
Some people think switching to orange juice is a workaround. It is-just not for all drugs. Fexofenadine (Allegra), an antihistamine, is actually less absorbed when taken with grapefruit or orange juice. That’s because those juices block a different transporter in the gut. So while orange juice won’t cause toxicity with most meds, it can make some drugs less effective. Always check.
What Should You Do?
If you’re on any prescription medication, here’s what to do:
- Check your labels: Since 2014, the FDA has required manufacturers to include grapefruit warnings on drug labels. Look for phrases like "avoid grapefruit juice" or "do not consume grapefruit products." About 76% of affected drugs have this warning.
- Talk to your pharmacist: Pharmacists are trained to catch these interactions. A 2021 study found 89% of community pharmacists screen for grapefruit interactions when filling prescriptions. Ask them directly: "Does this interact with grapefruit?" Don’t assume they’ll tell you unless you ask.
- Keep a full medication list: Include everything-prescription, over-the-counter, and supplements. Some herbal products and even vitamins can interact. Don’t forget things like St. John’s wort or high-dose vitamin C.
- Ask about alternatives: If you love grapefruit and you’re on simvastatin, ask your doctor about switching to pravastatin or rosuvastatin. If you’re on cyclosporine, ask about tacrolimus. Safe alternatives exist for many high-risk drugs.
- Be consistent: If you’re told to avoid grapefruit, avoid it completely-not just on days you take your pill. The enzyme block lasts for days. One glass on Monday can affect your Tuesday dose.
What Happens If You Accidentally Drink It?
If you had one glass and didn’t know, don’t panic. But do pay attention. Watch for unusual symptoms: muscle pain or weakness (especially with statins), dizziness, irregular heartbeat, nausea, confusion, or extreme fatigue. If you notice anything out of the ordinary, call your doctor or pharmacist. Don’t wait for a crisis.
There’s no antidote. The body has to regenerate the CYP3A4 enzyme, which takes 2-3 days. So if you drank grapefruit juice and you’re on a high-risk drug, skip your next dose only if your provider advises it. Never stop a medication on your own.
The Bigger Picture
Despite decades of research, patient awareness is shockingly low. A 2022 survey found only 38% of patients recalled being warned about grapefruit interactions when prescribed a risky medication. That’s not just a gap in education-it’s a public health risk.
Drug companies have lost over $1.2 billion annually in sales because patients quit taking simvastatin over grapefruit fears. That’s not because the drug doesn’t work-it’s because people don’t know what’s safe. Meanwhile, researchers are working on solutions. In October 2023, the USDA announced CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety tests. Maybe one day, you’ll be able to enjoy it without worry.
Until then, the safest rule is simple: if your medication warns against grapefruit, don’t take it. Not sometimes. Not "just a little." Not even if you think you’re fine. Your body doesn’t always tell you when something’s wrong-until it’s too late.

Esperanza Decor
November 12, 2025 AT 18:33This is one of those things that should be on every prescription bottle like a warning label. I had no idea grapefruit juice could mess with my meds like that. My grandma drinks it every morning with her statin, and I’m going to text her right now. This isn’t just a dietary quirk-it’s a silent killer.
Deepa Lakshminarasimhan
November 13, 2025 AT 03:40They say it’s the furanocoumarins, but what if it’s not the juice at all? What if it’s the pesticides sprayed on the fruit, or the plastic containers the juice comes in? They’ve been hiding this for decades to protect big pharma. I read a forum where someone said their doctor changed their med after they stopped drinking juice-but only after they switched to organic. Coincidence? I think not.
Erica Cruz
November 13, 2025 AT 10:09Let’s be real-this article reads like a pharmaceutical pamphlet dressed up as journalism. Statins are overprescribed anyway. If your body can’t handle grapefruit juice while on simvastatin, maybe you shouldn’t be on simvastatin in the first place. And let’s not pretend this is some groundbreaking revelation. I’ve known about this since 2010. Why is this even trending now?
Johnson Abraham
November 15, 2025 AT 01:44bro i just drank grapefruit juice with my blood pressure pill and now my heart feels weird… is it too late?? 😳
Shante Ajadeen
November 16, 2025 AT 12:06Thanks for laying this out so clearly. I’ve been on amlodipine for years and always wondered why my doctor said orange juice was fine but grapefruit wasn’t. Now I get it. I’ll pass this along to my mom-she’s 72 and drinks grapefruit juice with her pills. She needs to know.
dace yates
November 17, 2025 AT 21:08Wait-does this apply to grapefruit soda too? I’ve been drinking that instead of juice because I think it’s "healthier."
Danae Miley
November 19, 2025 AT 20:12No, grapefruit soda is irrelevant unless it contains actual grapefruit juice or extract. Most commercial sodas use artificial flavoring that lacks furanocoumarins. But you should still check the ingredient list-"natural flavors" can be deceptive. This isn’t a trivial distinction; misinformation kills.
Charles Lewis
November 20, 2025 AT 16:54It’s worth emphasizing that the danger isn’t just about the drug concentration-it’s about the cumulative, unpredictable effect on an aging, polypharmacy-prone population. We’re not talking about a single variable interaction. We’re talking about a systemic failure in patient education, compounded by the fact that many elderly patients rely on caregivers who themselves lack medical literacy. The FDA warning label requirement is a step, but insufficient. What we need is mandatory pharmacist counseling at point-of-dispense for high-risk medications, standardized patient handouts in plain language, and public health campaigns that don’t assume people read fine print. Until then, we’re leaving vulnerable people to guess their way through a minefield disguised as wellness.