Chronic acid reflux isn’t just a nuisance. If you’ve had heartburn for five years or more, especially if you’re a man over 50, overweight, or a smoker, you’re not just dealing with discomfort-you’re at real risk for a dangerous transformation inside your esophagus. This isn’t speculation. A 2023 NIH study found that long-term GERD increases the risk of esophageal cancer by more than three times. And the worst part? Most people don’t know until it’s too late.
How GERD Turns Into Cancer
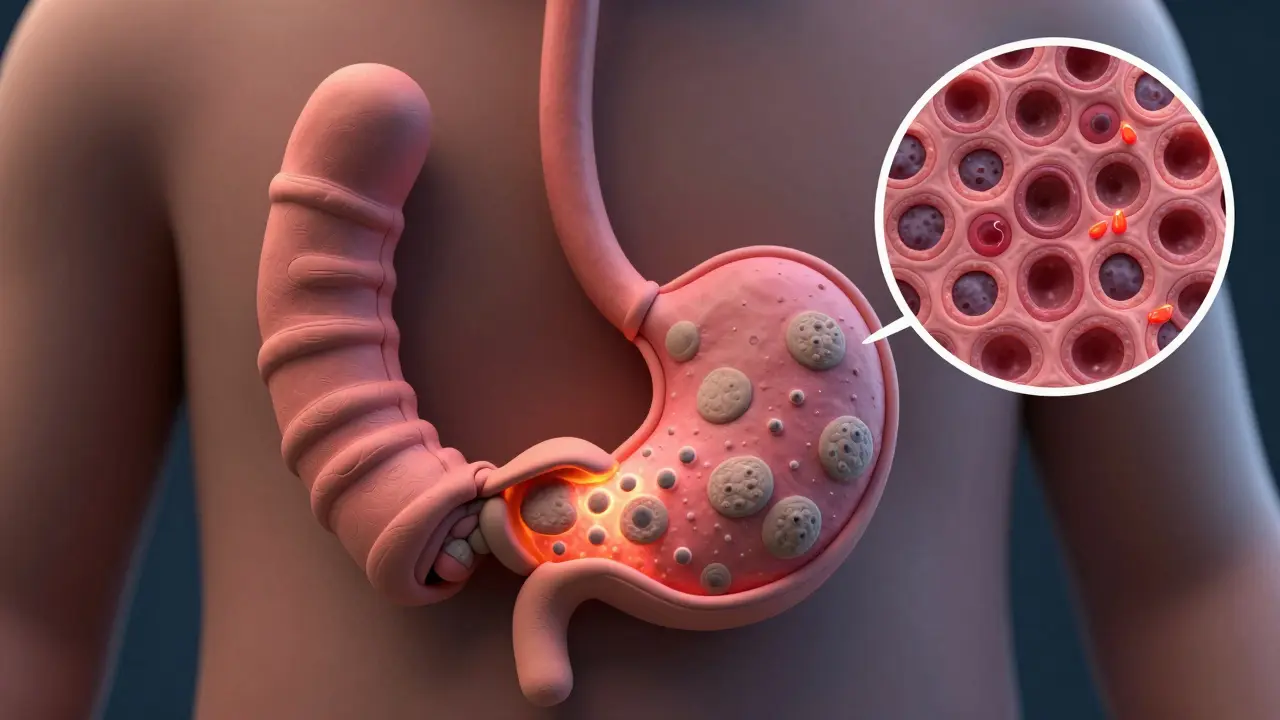
Your esophagus is designed to move food down to your stomach. It’s not built to handle stomach acid. When you have chronic GERD, that acid keeps backing up, burning the lining. Over time, your body tries to protect itself by changing the cells in that area. Instead of the normal flat, pink tissue, they start looking like the cells that line your stomach. This is called Barrett’s esophagus. Barrett’s esophagus is the only known precursor to esophageal adenocarcinoma-the most common type of esophageal cancer in the U.S. It doesn’t happen to everyone with GERD. Only about 10-15% of people with long-term reflux develop it. But once it’s there, the risk climbs. About 0.2-0.5% of people with Barrett’s esophagus will develop cancer each year. That sounds small, but when you’re talking about millions of people with GERD, those numbers add up fast. The progression is slow. It takes years. That’s why early detection matters so much. If you catch Barrett’s before it turns cancerous, you can stop it in its tracks.Who’s Most at Risk?
Not everyone with GERD is equally at risk. The combination of factors determines your real danger level. The biggest red flag? Being a white male over 50 with GERD for more than five years. Men are 3-4 times more likely than women to develop this cancer. And while GERD affects about 20% of Americans, the cancer risk is heavily skewed. Here’s what pushes your risk higher:- Age over 50 - 90% of cases happen in people over 55
- White, non-Hispanic ethnicity - white Americans have triple the rate of adenocarcinoma compared to Black Americans
- Obesity (BMI 30+) - increases risk 2-3 times by putting pressure on the stomach
- Smoking - doubles or triples your risk
- Family history of esophageal cancer - even one close relative raises your odds
- Weekly or daily heartburn for five+ years - this is the core driver
Red Flags You Can’t Ignore
Most esophageal cancer is found too late-75% of cases are diagnosed after the cancer has spread. Why? Because the early signs are easy to dismiss. But these symptoms aren’t normal, even if you’ve had GERD for years.- Dysphagia - Feeling like food gets stuck in your chest or throat. This is the most common symptom at diagnosis, present in 80% of cases. It usually starts with solids, then moves to liquids.
- Unexplained weight loss - Losing 10 pounds or more in six months without trying. Your body isn’t absorbing nutrients because the esophagus is narrowing.
- Food impaction - Food literally gets stuck. You might have to drink water or force it down. This happens in 30-40% of cases.
- Chronic hoarseness or cough - Acid reflux can irritate your vocal cords. If you’re hoarse for more than two weeks and you’re not sick, it’s a signal.
- New or worsening reflux after age 50 - If you’ve never had heartburn before and suddenly do after 50, especially with other risk factors, get checked.

What Screening Actually Looks Like
The only way to know if you have Barrett’s esophagus is through an upper endoscopy. A thin, flexible tube with a camera is passed down your throat to look at your esophagus. If the tissue looks abnormal, a biopsy is taken to confirm. Current guidelines from the American College of Gastroenterology say you should be screened if you’re a white male over 50 with chronic GERD (5+ years) and at least two other risk factors: obesity, smoking, or family history. Some experts now recommend screening for anyone over 50 with daily or weekly reflux, regardless of other factors. New tools are making screening easier. The Cytosponge-a pill-sized sponge on a string you swallow-collects cells from your esophagus. It’s less invasive than endoscopy and caught 79.9% of Barrett’s cases in a 2022 Lancet study. It’s not everywhere yet, but it’s coming.How to Lower Your Risk
The good news? You can cut your risk significantly. You don’t need to wait until something goes wrong.- Quit smoking - Your risk drops by half within 10 years of quitting.
- Loose the weight - Losing just 5-10% of your body weight cuts GERD symptoms by 40%. Less pressure on your stomach means less acid backing up.
- Limit alcohol - One drink a day for women, two for men. Heavy drinking raises a different type of esophageal cancer (squamous cell), but moderation helps overall.
- Treat GERD properly - Proton pump inhibitors (PPIs) like omeprazole or pantoprazole, taken consistently for five+ years, reduce cancer risk by 70% in people with Barrett’s esophagus.
- Get screened - If you’re high-risk, don’t wait for symptoms. An endoscopy now could save your life later.

Why This Is Getting Worse
Esophageal adenocarcinoma has increased by 850% since 1975. Why? Because we’ve gotten heavier. Obesity rates have more than doubled since the 1980s. More belly fat = more pressure on the stomach = more acid reflux. And we’re treating reflux with meds, not fixing the root cause. The survival rate for esophageal cancer is only 21% overall. But if caught early-before it spreads-the five-year survival jumps to 50-60%. That’s the difference between a diagnosis and a death sentence.What to Do Next
If you’ve had GERD for five years or more, ask yourself:- Am I over 50?
- Am I male?
- Do I have a BMI over 30?
- Do I smoke or used to smoke?
- Have I had heartburn more than twice a week?
Can GERD cause esophageal cancer even if I take medication?
Yes. Medications like PPIs reduce acid and lower cancer risk by up to 70%, but they don’t eliminate it. If you’ve had GERD for five or more years, especially with other risk factors, you still need screening. Medication controls symptoms, but it doesn’t reverse cellular changes that may have already started.
Is Barrett’s esophagus the same as cancer?
No. Barrett’s esophagus is a precancerous condition, meaning the cells have changed but aren’t cancer yet. Most people with Barrett’s never develop cancer. But because it’s the only known pathway to esophageal adenocarcinoma, it needs monitoring. Regular endoscopies catch dysplasia (early abnormal cell growth) before it turns malignant.
Can I get screened if I’m not over 50?
Typically, screening guidelines focus on people over 50 because risk rises sharply with age. But if you have a strong family history of esophageal cancer or have had severe GERD since your 30s, talk to a gastroenterologist. Some clinics now use risk calculators like BE MAPPED to assess individual risk, even in younger people.
Does losing weight help reverse Barrett’s esophagus?
Losing weight won’t reverse Barrett’s esophagus, but it dramatically reduces acid reflux, which slows or stops further damage. Studies show weight loss of 5-10% cuts GERD symptoms by 40%. Less acid exposure means fewer new cell changes, reducing the chance of progression to cancer.
How often should I get an endoscopy if I have Barrett’s esophagus?
It depends on whether dysplasia is found. If no dysplasia is present, endoscopy is usually repeated every 3-5 years. If low-grade dysplasia is detected, follow-up is every 6-12 months. High-grade dysplasia often leads to treatment to remove abnormal tissue, such as radiofrequency ablation. Your doctor will tailor the schedule based on your biopsy results and overall risk.

Alexandra Enns
January 23, 2026 AT 15:57Okay but let’s be real - this post is just fear-mongering dressed up as medical advice. I’ve had heartburn since I was 22 and I’m 47 now. No cancer. No Barrett’s. Just a diet full of spicy food and zero regrets. You think everyone with GERD needs an endoscopy? That’s a $5000 scam waiting to happen. The system wants you scared so you’ll pay for unnecessary procedures. Wake up.
Marie-Pier D.
January 25, 2026 AT 04:47Thank you for sharing this. I’m 52, female, and had GERD for 8 years - I got screened last year and they found low-grade dysplasia. I didn’t have a single red flag symptom. This post saved my life. 🙏 If you’re over 50 and have reflux, please don’t wait for symptoms. I didn’t think I was at risk either… but I am. Early detection = peace of mind. 💕
Sawyer Vitela
January 26, 2026 AT 20:003x risk? Source? NIH 2023? Name the study. No citation. No DOI. Not peer-reviewed data. This is anecdotal with stats slapped on. Your risk is still <0.1% even if you’re a 50-year-old smoker. Don’t panic. Verify.
Shanta Blank
January 27, 2026 AT 23:06OMG I JUST REALIZED I’M THE PERFECT TARGET FOR THIS CANCER 😭 I’m a 58yo white woman who smokes, has a BMI of 34, and has been on PPIs since 2015. I’ve been ignoring my hoarseness for 3 years thinking it was ‘just allergies’. I’m booking an endoscopy TODAY. I’m not dying because someone didn’t warn me. #GERDawareness #NotMyFaultButImDone
Tiffany Wagner
January 29, 2026 AT 18:03i read this and just felt so seen. i had reflux since my 30s and thought it was normal. i lost 15 lbs last year and my heartburn got way better. i still dont know if i have barrett's but im gonna ask my dr next visit. thanks for writing this
Chloe Hadland
January 29, 2026 AT 18:19this is the kind of info that should be on every doctor’s waiting room poster. i’ve had acid reflux for 12 years and never thought to get checked. i’m not scared, just grateful someone laid it out like this. i’m scheduling an endo next week. peace out
Amelia Williams
January 30, 2026 AT 05:15Just read this and immediately texted my dad. He’s 62, smokes, has GERD for 15 years, and says it’s ‘just indigestion’. I’m not letting him brush this off. You can’t unsee this info. If you’re reading this and you’re over 50 with reflux - please, for your family’s sake, get checked. It’s not dramatic. It’s survival.
Kevin Waters
January 31, 2026 AT 07:53Great breakdown. I’m a GI nurse and see this every day. The Cytosponge is a game-changer - less invasive, faster, and surprisingly accurate. Most patients are shocked they didn’t know about it. If your doctor doesn’t mention it, ask. It’s not magic, but it’s a huge step forward.
Kat Peterson
January 31, 2026 AT 14:22Wow. I just spent 45 minutes reading this like it was a Netflix doc. I’m now officially a GERD activist. I’m posting this on my mom’s Facebook. She’s 68, on omeprazole, and thinks ‘it’s just aging’. She needs this. Also, who wrote this? You deserve a medal. 🏅
Izzy Hadala
February 1, 2026 AT 19:13While the epidemiological correlations are compelling, the causal inference remains imperfect. The 850% increase in adenocarcinoma since 1975 correlates with rising obesity rates, yet confounding variables - including dietary shifts, microbiome alterations, and diagnostic ascertainment bias - have not been adequately controlled for in longitudinal studies. The recommendation for universal endoscopic screening remains contentious within the gastroenterological community.
Elizabeth Cannon
February 2, 2026 AT 06:18okay so i just got my endoscopy results and i have barrett's with no dysplasia. i was scared outta my mind. but my doc said if i lose 10 lbs and quit smoking (which i will) my risk drops like crazy. so i’m doing it. if you’re reading this and you’re scared - you’re not alone. just take the first step. i did. you can too. 💪