DOAC Dosing Calculator for Kidney & Liver Disease
This tool calculates appropriate dosing for direct oral anticoagulants (DOACs) based on kidney function and liver disease severity. Always consult a physician for clinical decisions.
Why Blood Thinners Get Complicated with Kidney or Liver Disease
When your kidneys or liver aren’t working right, taking a blood thinner becomes a high-wire act. You need to prevent clots-like strokes or lung clots-but too much thinning can cause dangerous bleeding. This isn’t theoretical. In the U.S., nearly 40 million people have chronic kidney disease, and almost 6 million have chronic liver disease. Many of them also have atrial fibrillation, which makes anticoagulation necessary. But here’s the problem: most clinical trials that tested newer blood thinners (DOACs) excluded people with severe kidney or liver damage. So doctors are flying blind in real life.
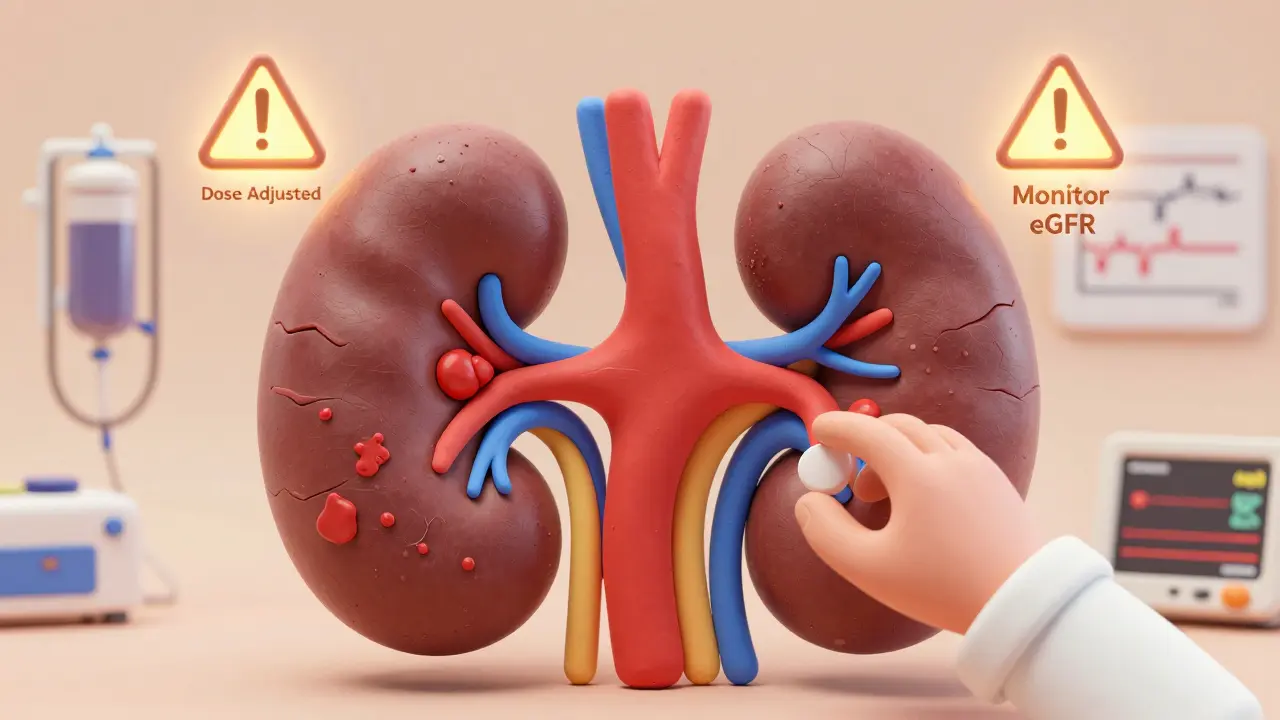
How Kidney Disease Changes the Rules for Blood Thinners
Your kidneys clear most blood thinners from your body. When they fail, the drug builds up. That’s why dose adjustments aren’t optional-they’re life-or-death.
For mild to moderate kidney disease (eGFR 45+), standard DOAC doses are usually fine. But once eGFR drops below 45, things get tricky. Apixaban is the most forgiving. Even at eGFR 25-30, it’s still safer than warfarin. In fact, the ARISTOTLE trial showed apixaban cut major bleeding by 70% compared to warfarin in this group. Rivaroxaban and edoxaban need dose reductions at eGFR 30-49. Dabigatran? Avoid it completely if eGFR is under 30-it’s cleared 80% by the kidneys, so it piles up fast.
For patients on dialysis, the data is messy. Some studies show apixaban 2.5 mg twice daily works okay. Others show bleeding risks spike. The European guidelines say don’t use DOACs in dialysis patients. The American guidelines say maybe, if you pick apixaban and monitor closely. Why the split? Because no large randomized trial has been done. The MYD88 trial, which should give clearer answers, won’t finish until 2025.
Warfarin is still used in dialysis patients-about 63% of treated cases in one big registry. But it’s not safer. INR levels fluctuate wildly in kidney failure, making it hard to keep the dose right. Many patients spend less than half their time in the safe range. And if they bleed? Reversal is slow and messy.
Liver Disease: It’s Not Just About INR
People assume liver disease means high INR, so they think the blood is already thin. That’s wrong. The liver makes both clotting and anti-clotting proteins. In cirrhosis, it makes less of both. So you’re not ‘naturally anticoagulated’-you’re just unstable.
Child-Pugh score is the go-to tool. Child-Pugh A (mild disease)? DOACs can be used normally. Child-Pugh B (moderate)? Use caution. Reduce the dose. Child-Pugh C (severe)? Don’t use DOACs. The RE-CIRRHOSIS study found these patients had over five times the risk of major bleeding on DOACs.
Here’s the kicker: INR doesn’t tell you the full story. It only measures vitamin K-dependent factors. In advanced liver disease, you also have low platelets, poor fibrinogen, and dysfunctional clotting. A normal INR can still mean you’re at high bleeding risk. That’s why some centers use TEG or ROTEM-tests that show how the whole clotting system behaves. But only 38% of U.S. hospitals have them.
Warfarin? It’s not the answer either. In cirrhosis, patients spend only 45% of their time in the therapeutic range-compared to 65% in healthy people. That means more clots, more bleeds, more trips to the ER.

Apixaban vs. Warfarin: The Real Numbers
Let’s cut through the noise. When you compare apixaban and warfarin in patients with kidney or liver disease, the data favors apixaban.
- In CKD stage 3-4, apixaban reduces major bleeding by 31% compared to warfarin.
- For intracranial bleeding (the deadliest kind), DOACs cut the risk by 62% in kidney disease patients.
- In dialysis patients, one study found DOACs had 14.2 bleeding events per 100 patient-years versus 18.7 for warfarin.
- But here’s the catch: stroke rates were nearly identical. So you’re not trading one risk for another-you’re trading a more predictable risk for a messier one.
Apixaban’s advantage comes down to pharmacology. Only 27% is cleared by the kidneys. That means even with failing kidneys, it doesn’t build up as badly as dabigatran (80%) or edoxaban (50%). Rivaroxaban is 33% renal, but it’s still not recommended in severe CKD because of GI bleeding risks.
What Happens When You Bleed? Reversal Is Harder Than You Think
Reversing warfarin? You give vitamin K and fresh frozen plasma. It’s old-school, but it works.
Reversing DOACs? You need special drugs. Andexanet alfa reverses apixaban and rivaroxaban-but it costs $19,000 per dose and only 45% of U.S. hospitals stock it. Idarucizumab reverses dabigatran at $3,500 per dose, but it’s useless for everything else. And if you’re on apixaban and your kidney function is terrible? The drug sticks around longer, so reversal takes longer.
Many hospitals don’t have protocols for dual organ failure. A 2021 survey found 78% of U.S. hospitals lack written guidelines for anticoagulating patients with both kidney and liver disease. That’s why medication errors are 3.2 times higher in this group.
Real Stories from the Front Lines
A nephrologist in Ohio treated 15 dialysis patients on apixaban 2.5 mg daily for two years. No bleeds. No strokes. Another in Chicago had a patient on the same dose suffer a massive retroperitoneal bleed. Both were on the same drug, same dose. What changed? Maybe it was diet. Maybe it was an infection. Maybe it was just bad luck.
In liver clinics, hepatologists report bleeding events almost every year. One doctor said, “I stopped giving DOACs to anyone with platelets under 70,000.” Another said, “I only use warfarin if the patient has portal vein thrombosis-it’s a bigger threat than bleeding.”
There’s no one-size-fits-all. It’s about balancing risk, not following a checklist.
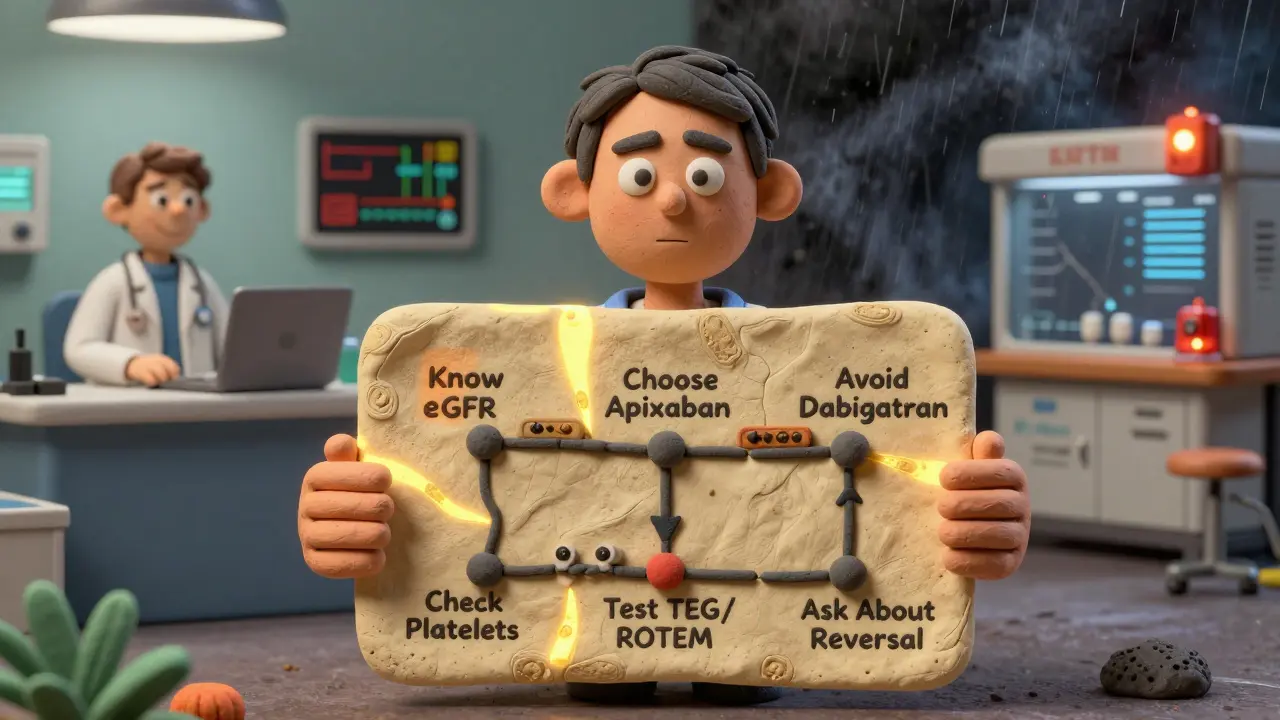
What Should You Do? A Practical Roadmap
- Know your eGFR and Child-Pugh score. If you’re on a blood thinner and have kidney or liver disease, ask your doctor for these numbers. Don’t assume they’re tracking them.
- Apixaban is usually the best bet. If you have moderate kidney disease (eGFR 25-44) or mild liver disease (Child-Pugh A), apixaban 2.5 mg twice daily is the most studied and safest option.
- Avoid dabigatran in kidney disease. It’s cleared mostly by the kidneys. Even mild CKD can make it dangerous.
- Don’t trust INR alone in liver disease. If you have cirrhosis and are on warfarin, ask about TEG or ROTEM testing. If your hospital doesn’t offer it, push for a referral.
- Monitor every 3 months. If your eGFR drops more than 5 points per year, your dose may need adjustment. Platelets under 50,000? Stop DOACs.
- Ask about the reversal plan. If you’re on apixaban, ask: “What do we do if I bleed?” If the answer is “We’ll call a specialist,” that’s not enough.
The Bottom Line
There’s no perfect answer. But there is a best path forward. Apixaban, at reduced doses, is the most reliable option for most patients with moderate kidney or liver disease. Warfarin is still used, but it’s harder to manage and carries higher bleeding risks. DOACs aren’t magic-they’re tools. And like any tool, they need the right context.
Doctors aren’t ignoring you. They’re wrestling with incomplete data. But that doesn’t mean you should accept uncertainty. Ask questions. Push for testing. Know your numbers. And if your doctor says, “We don’t know,” ask: “What’s the plan if things go wrong?” That’s the difference between just surviving-and truly being cared for.
Can I take apixaban if I’m on dialysis?
Some doctors prescribe apixaban 2.5 mg twice daily for dialysis patients with atrial fibrillation, especially if they’ve had bleeding on warfarin. But this is off-label and not FDA-approved. There’s no large trial proving it’s safe or effective. The European guidelines say no. The American guidelines say maybe. If you’re on dialysis, your doctor should weigh your stroke risk (CHA₂DS₂-VASc score) against your bleeding risk and monitor you closely.
Is warfarin safer than DOACs for liver disease?
Not necessarily. Warfarin has known reversal agents, but in advanced liver disease, INR is unreliable. Patients spend less time in the safe range, increasing both clot and bleed risks. DOACs aren’t recommended in Child-Pugh C, but in Child-Pugh A or B, apixaban may be safer than warfarin because it doesn’t rely on liver metabolism as much. The key is not the drug-it’s how well you can monitor and respond to changes.
Why can’t I just take a lower dose of rivaroxaban or edoxaban?
Rivaroxaban and edoxaban are cleared more by the liver than the kidneys, but they still carry higher bleeding risks in advanced disease. Rivaroxaban has been linked to 2.8 times more GI bleeding than warfarin in dialysis patients. Edoxaban’s data is even scarcer. Apixaban has the most safety data in this group. Lowering the dose of other DOACs doesn’t fix the underlying risk-it just delays the problem.
Should I get my platelet count checked regularly if I have cirrhosis?
Yes. In cirrhosis, low platelets (under 150,000) are common. But if your count drops below 50,000, the risk of bleeding spikes. Many hepatologists stop anticoagulants at that point. Monthly platelet checks are standard for anyone on blood thinners with liver disease. If your platelets are falling fast, your doctor may need to reconsider your anticoagulation plan.
What if my doctor won’t prescribe any blood thinner?
That’s common. About 70% of dialysis patients with atrial fibrillation aren’t on anticoagulants-even though most have high stroke risk. But if your CHA₂DS₂-VASc score is 3 or higher, you’re at real risk. Ask if apixaban at 2.5 mg twice daily is an option. If your doctor refuses, ask for a cardiology or hematology consult. You deserve a full risk assessment-not just avoidance.

Siobhan Goggin
January 3, 2026 AT 18:01John Wilmerding
January 4, 2026 AT 21:12That said, we avoid it entirely if platelets drop below 50k or if there's active GI bleeding. The data isn't perfect, but it's better than warfarin's wild INR swings.
Also, never underestimate the role of diet - high potassium meals can delay apixaban clearance in renal failure. Simple things matter.
John Ross
January 6, 2026 AT 18:16Let’s be real: we’re trading convenience for catastrophe. The real problem isn’t the drugs - it’s the system that rewards speed over safety. And now we’re teaching residents that ‘apixaban is safer’ without teaching them how to recognize early signs of hemorrhage in cirrhotic patients. That’s malpractice by protocol.
Allen Ye
January 7, 2026 AT 17:59Here, a patient with cirrhosis and CKD is bounced between nephrology, hepatology, and cardiology - each specialist prescribing based on their own siloed data. No one has the full picture. No one has the time. And the patient? They're the one who ends up in the ER with a retroperitoneal bleed, and suddenly everyone's scrambling to figure out what was given and why.
This isn't a pharmacology problem. It's a healthcare infrastructure problem. We've outsourced complexity to algorithms and guidelines that were never meant for real-world chaos.
Vikram Sujay
January 9, 2026 AT 03:52Apixaban is not inherently safer - it is merely less studied in extremes. Warfarin is not inherently worse - it is merely harder to manage. The difference lies not in the molecules, but in our willingness to accept uncertainty.
Perhaps the real question is not which drug to choose, but whether we, as physicians, are prepared to sit with the ambiguity - to monitor, to adapt, to admit we do not know - rather than reach for the illusion of control through standardized protocols.
Jay Tejada
January 10, 2026 AT 11:38Meanwhile, the patient’s daughter is Googling ‘apixaban dialysis bleeding’ at 2 a.m. and finds a 2019 case report of a guy who died from a brain bleed on the same dose.
Y’all are just winging it with billion-dollar pharma marketing as your guide. I’m not mad. I’m just disappointed.
Shanna Sung
January 12, 2026 AT 06:46mark etang
January 13, 2026 AT 05:16