Drug Absorption Interaction Checker
Check if Your Medication is Affected
Enter your medication to see if stomach acidity changes could reduce absorption. This tool helps you identify potential interactions with proton pump inhibitors (PPIs) and H2 blockers.
Enter a medication name to check for potential interactions with acid-reducing drugs.
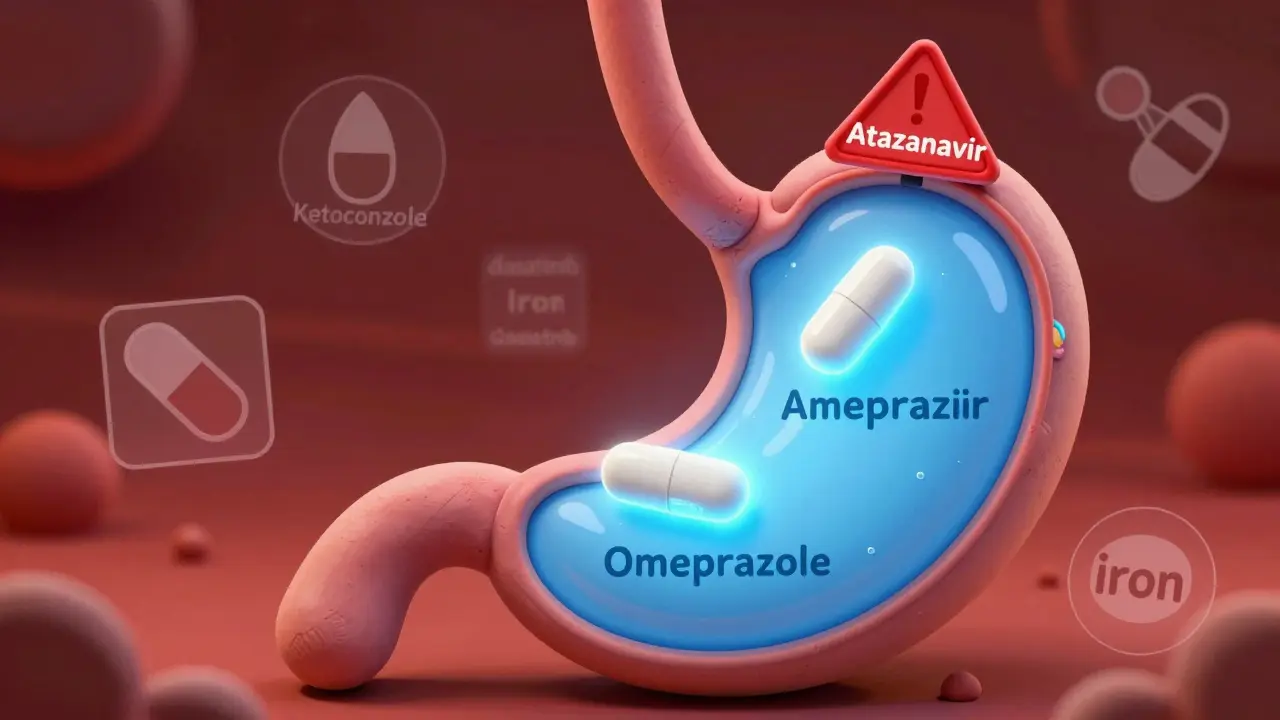
When you take a proton pump inhibitor like omeprazole or an H2 blocker like famotidine for heartburn, you’re not just changing your stomach’s acidity-you’re changing how your body absorbs other medications. This isn’t theoretical. It’s happening right now to millions of people who don’t realize their heartburn medicine is quietly sabotaging their blood pressure pills, antifungals, or even HIV treatment.
How Acid-Reducing Medications Work
Proton pump inhibitors (PPIs) and histamine H2-receptor antagonists (H2RAs) reduce stomach acid by targeting different parts of the acid-production system. PPIs like omeprazole, pantoprazole, and esomeprazole permanently block the proton pumps in stomach cells. H2RAs like ranitidine and famotidine block histamine signals that tell those cells to make acid. Both raise gastric pH from its normal level of 1.0-3.5 up to 4.0-6.0. That sounds harmless, even helpful-until you realize that many drugs need that acidic environment to dissolve properly.
The Science Behind Drug Absorption
Most oral drugs are either weak acids or weak bases. Their ability to dissolve-and be absorbed-depends heavily on pH. Weak bases like atazanavir (an HIV drug) or dasatinib (a leukemia treatment) need an acidic stomach to become soluble. In low pH, they turn into charged molecules that dissolve easily. When PPIs raise the pH, these drugs stay neutral and don’t dissolve well. The result? Less of the drug enters your bloodstream.
Studies show atazanavir’s absorption drops by up to 95% when taken with a PPI. That’s not a small drop-it’s enough to cause viral rebound in HIV patients. One Reddit user reported their viral load jumped from undetectable to 12,000 copies/mL after starting omeprazole. Their infectious disease specialist confirmed: this is a textbook interaction.
Weak acids like aspirin behave the opposite way-they absorb better in higher pH. But these interactions are usually minor, rarely causing clinical issues. The real danger lies with weak bases that have narrow therapeutic windows. A small change in absorption can mean the difference between treatment success and complete failure.
Which Drugs Are Most Affected?
The FDA identifies at least 15 commonly prescribed drugs with clinically significant interactions with acid-reducing medications. The worst offenders include:
- Atazanavir: HIV protease inhibitor. PPIs reduce absorption by 74-95%. Do not combine.
- Dasatinib: Leukemia drug. Absorption drops by 60%. Dose adjustments or staggered timing may help.
- Ketoconazole: Antifungal. Absorption drops 75%. Often becomes completely ineffective.
- Nilotinib: Another leukemia drug. Similar pattern to dasatinib.
- Erlotinib: Lung cancer drug. Reduced absorption linked to lower response rates.
Even drugs you wouldn’t suspect-like mycophenolate (used after organ transplants) or iron supplements-are affected. Iron needs acid to convert into its absorbable form. PPIs can cause iron deficiency even when patients take supplements.

PPIs vs. H2 Blockers: Not All Are Equal
Not all acid reducers are created equal when it comes to drug interactions. PPIs are far more dangerous than H2RAs. Why? Because they work harder and longer.
PPIs keep stomach pH above 4 for 14-18 hours a day. H2RAs only do it for 8-12 hours. A 2024 JAMA Network Open study found PPIs reduce absorption of pH-dependent drugs by 40-80%, while H2RAs reduce it by 20-40%. That’s a huge difference.
Also, immediate-release formulations are more vulnerable than extended-release versions. And enteric-coated pills? They’re designed to dissolve in the intestine-but if stomach pH rises too high, they can dissolve too early, breaking down in the stomach instead of the intestine. That can cause irritation or destroy the drug before it’s absorbed.
Real-World Consequences
This isn’t just a lab phenomenon. In a 2023 study of over 12,500 patients, those taking dasatinib with a PPI had 37% higher rates of treatment failure. That means more relapses, more hospitalizations, more cancer progression.
The FDA’s adverse event database recorded 1,247 reports of therapeutic failure linked to acid-reducing drugs between 2020 and 2023. Atazanavir led the list with 312 reports. Dasatinib came second with 287. Ketoconazole followed with 198.
One Drugs.com user wrote: “My doctor didn’t tell me Nexium would interfere with my blood pressure meds. My readings were consistently 20 points higher until we figured out the interaction.”
And it’s not just about effectiveness. Some patients end up taking higher doses of their main medication-thinking it’s not working-when the real problem is the PPI blocking absorption. That increases side effects and risk.
What Can You Do?
There are practical ways to manage these interactions-without giving up acid control entirely.
- Stagger doses. Take the affected drug at least 2 hours before the acid reducer. For dasatinib, studies show this restores about 85% of effectiveness when timed correctly.
- Switch to an H2 blocker. If you need long-term acid control, famotidine may be safer than pantoprazole. But even H2RAs aren’t risk-free.
- Use antacids occasionally. Calcium carbonate or magnesium hydroxide can neutralize acid temporarily. Take them 2-4 hours apart from your other meds. But they don’t last long-so they’re not good for daily use.
- Ask about alternatives. Is the PPI even necessary? The American College of Gastroenterology says 30-50% of long-term PPI users don’t have a valid reason to be on them. Deprescribing can prevent dozens of drug interactions.

Pharmacists Are Your Secret Weapon
Most doctors don’t memorize every drug interaction. But pharmacists do. A 2023 study showed pharmacist-led medication reviews cut inappropriate ARA co-prescribing by 62% in Medicare patients.
When you pick up a new prescription, ask: “Could this interact with my heartburn medicine?” If your pharmacist says yes, they can often suggest a safer alternative or timing strategy.
Electronic health records now flag these interactions. Epic Systems reports 78% of doctors follow the alerts. But alerts aren’t perfect. If you’re on multiple meds, it’s still your job to ask.
The Bigger Picture
Over 15 million Americans take PPIs daily. Many have been on them for years-even when they only need them for a few weeks. The FDA and European Medicines Agency now require 28 drug labels to warn about ARA interactions, up from just 12 five years ago.
This isn’t just a medical issue-it’s a financial one. Wasted drugs, failed treatments, and hospitalizations cost the U.S. healthcare system $1.2 billion a year.
Pharmaceutical companies are responding. Nearly 40% of new drugs in development now include pH-independent delivery systems to avoid these problems. AI tools are being trained to predict interactions with 89% accuracy. And research into personalized gastric pH monitoring could soon let doctors tailor acid-reducing therapy to your individual needs.
For now, the best defense is awareness. If you’re on a PPI or H2 blocker and also take any other medication, especially for HIV, cancer, or heart disease, talk to your pharmacist. Don’t assume your doctor knows. Don’t assume your meds are safe together. And don’t stop your acid reducer without guidance-but do question whether you really need it.
Can I still take a PPI if I’m on atazanavir?
No. Combining atazanavir with a proton pump inhibitor can reduce its absorption by up to 95%, leading to HIV treatment failure and drug resistance. The FDA and drug manufacturers explicitly warn against this combination. If you need acid control, your doctor may switch you to an H2 blocker like famotidine or use antacids with strict timing, but PPIs are contraindicated.
Do H2 blockers like famotidine cause the same problems as PPIs?
H2 blockers like famotidine and ranitidine raise stomach pH less and for a shorter time than PPIs, so their interaction risk is lower-typically 20-40% reduction in absorption versus 40-80% with PPIs. They’re often a safer alternative for patients who need acid control while taking drugs like dasatinib or ketoconazole. But they’re not risk-free. Always check with your pharmacist before combining them with other medications.
How do I know if my medication is affected by acid reducers?
Check the drug’s prescribing information for warnings about “gastric pH,” “acid-reducing agents,” or “PPIs.” Medications that are weak bases (pKa >7) with low solubility at higher pH are most at risk. Common examples include atazanavir, dasatinib, ketoconazole, erlotinib, and iron supplements. If you’re unsure, ask your pharmacist to run a drug interaction check using your full list of medications.
Can I just take my PPI and my other drug at different times of day?
Timing helps-but it’s not a full solution. Taking a weak base drug like dasatinib 2 hours before a PPI can restore about 85% of its absorption in some cases. But because PPIs work for 14-18 hours, the stomach remains less acidic all day. This only reduces the interaction by 30-40%. It’s better than nothing, but not reliable for drugs with narrow therapeutic windows like atazanavir.
Why aren’t doctors always warning patients about this?
Many doctors aren’t aware of the full scope of these interactions, especially if they’re not specialists. PPIs are often prescribed for short-term use, and the long-term risks aren’t always discussed. Also, patients rarely mention their OTC heartburn meds unless asked. That’s why pharmacist-led reviews are so effective-they catch these hidden combinations. Always tell your provider about every pill, supplement, and OTC drug you take-even if you think it’s harmless.
What’s Next?
The future of drug delivery is moving away from pH-dependent absorption. New formulations are being designed to work regardless of stomach acidity. AI tools are getting better at predicting which combinations are dangerous. And deprescribing initiatives are helping patients stop PPIs they don’t need.
But until then, the most powerful tool you have is information. Know your meds. Ask questions. Talk to your pharmacist. And don’t assume that because something is common-like a PPI for heartburn-it’s safe with everything else you take.

Susie Deer
January 15, 2026 AT 05:40TooAfraid ToSay
January 17, 2026 AT 05:00Henry Sy
January 17, 2026 AT 05:03shiv singh
January 17, 2026 AT 15:54Robert Way
January 19, 2026 AT 00:41Sarah Triphahn
January 20, 2026 AT 02:52Allison Deming
January 20, 2026 AT 23:10Dylan Livingston
January 21, 2026 AT 08:55Andrew Freeman
January 22, 2026 AT 23:17says haze
January 24, 2026 AT 18:59Alvin Bregman
January 26, 2026 AT 08:36Sarah -Jane Vincent
January 27, 2026 AT 11:38Anna Hunger
January 28, 2026 AT 04:16