For decades, cancer treatment meant one thing: chemotherapy. Harsh, broad, and often debilitating. But today, a quiet revolution is happening in oncology. Instead of attacking all fast-growing cells, doctors now look at the unique genetic fingerprint of a tumor. This is targeted therapy - a smarter, more precise way to fight cancer.
What Exactly Is Targeted Therapy?
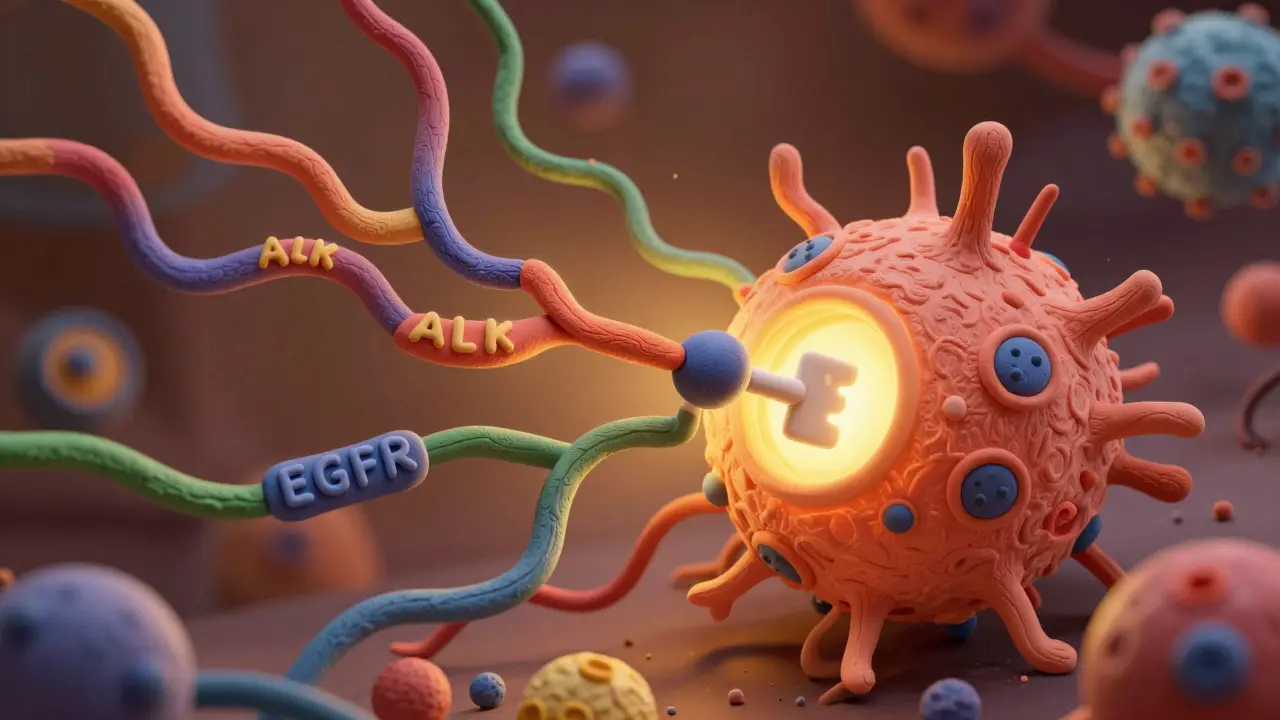
Targeted therapy isn’t about killing cells randomly. It’s about finding the exact molecular mistake that’s making a cancer grow - and then hitting it with a drug designed for that one flaw. Think of it like using a key to unlock a specific lock. If the tumor has a mutation in the EGFR gene, you use a drug that blocks EGFR. If it has an ALK fusion, you use an ALK inhibitor. The goal? Destroy the cancer while leaving healthy tissue mostly untouched.
This approach didn’t appear out of nowhere. It was built on the foundation of The Cancer Genome Atlas (TCGA), a massive project that mapped genetic changes in over 20,000 tumors across 33 cancer types. Before TCGA, we treated lung cancer, colon cancer, and breast cancer as separate diseases. Now we know that a lung tumor with an NTRK fusion behaves more like a rare salivary gland tumor with the same mutation than like a typical lung cancer. That’s why drugs like larotrectinib can work across different cancer types - as long as the genetic target is there.
How Do These Drugs Work?
There are two main types of targeted therapies: small molecule inhibitors and monoclonal antibodies.
Small molecule drugs, like osimertinib for EGFR-mutant lung cancer, are tiny enough to slip inside cells. They block the signals that tell cancer to grow. Osimertinib doesn’t just shrink tumors - in clinical trials, it doubled the time patients lived without their cancer worsening compared to older chemo drugs.
Monoclonal antibodies, like trastuzumab for HER2-positive breast cancer, work from the outside. They latch onto proteins on the surface of cancer cells. Once attached, they either flag the cell for immune destruction or block growth signals directly. These drugs often come with fewer side effects than chemo - no hair loss, less nausea, and often no need for hospital visits.
But here’s the catch: these drugs only work if the tumor has the right mutation. That’s why testing is non-negotiable.
Why Genetic Testing Is the First Step
Before any targeted therapy is given, doctors need to know what they’re targeting. That means testing the tumor’s DNA. The standard tool today is next-generation sequencing (NGS), which scans hundreds of cancer-related genes at once. Tests like FoundationOne CDx or MSK-IMPACT look at 300-500 genes and can spot mutations, fusions, and other abnormalities in a single sample.
But it’s not simple. The test needs enough tumor tissue - at least 20-50 nanograms of DNA with 20% cancer cells. If the sample is too small or too old, results can be unreliable. Turnaround time? Two to three weeks. That’s a long wait when you’re fighting cancer.
And not every mutation means a treatment exists. Only about 13.8% of cancer patients have a mutation that matches an approved targeted drug. Even among those who do, resistance often develops. In 70-90% of cases, the cancer finds a way around the drug within a year. That’s why researchers are now testing combinations - pairing targeted drugs with immunotherapy or other inhibitors to delay resistance.

Real Results: Numbers That Matter
Let’s talk outcomes. For patients with EGFR-mutant non-small cell lung cancer, osimertinib extends progression-free survival to nearly 19 months - almost double what chemo offers. In melanoma with BRAF V600E mutations, combination therapy with dabrafenib and trametinib can keep the disease under control for over two years.
For rare cancers with NTRK fusions, larotrectinib achieves a 75% response rate - no matter where the tumor started. That’s why the FDA approved it as a tissue-agnostic treatment. It’s not about where the cancer is - it’s about what’s driving it.
And toxicity? Big win. Only 15-30% of patients on targeted therapy experience severe side effects, compared to 50-70% with traditional chemo. Many patients report feeling well enough to work, travel, or care for their families.
The Hidden Challenges
But this isn’t a magic bullet. For every success story, there’s a frustrating one.
First, cost. A single month of targeted therapy can run $15,000 to $30,000. Insurance often denies coverage - especially for off-label use or rare mutations. One patient on Reddit wrote: “My NTRK fusion makes me eligible for larotrectinib, but my insurance denied it because it’s ‘not standard for my cancer type.’” That’s not rare. In a 2022 survey, 55% of patients said they faced insurance delays for genomic testing.
Second, access. In the U.S., 65% of advanced cancer patients get genomic testing. In Europe, it’s 22%. In parts of Asia, it’s under 10%. Even in major U.S. hospitals, only 32% of community centers offer comprehensive testing. Many oncologists don’t have the training to interpret complex genetic reports. A 2023 ASCO survey found institutional reports scored just 2.8 out of 5 for clarity - while commercial reports scored 4.2.
Third, not all mutations are treatable. Targeted drugs work best on “oncogene addiction” - when a tumor relies on one broken gene. But 80% of driver mutations are in tumor suppressor genes like TP53 or PTEN. We still have no drugs to fix these. We can’t turn a broken brake pedal back on - only slow the car down.

Who Benefits the Most?
Targeted therapy isn’t for everyone. It works best in:
- Patients with advanced or metastatic cancer
- Those whose tumors have been tested and show a known actionable mutation
- People who can tolerate the wait for genetic results
- Those with access to specialized care and insurance coverage
It’s less effective for early-stage cancers, where surgery or radiation may still be the best option. And it’s rarely used as a first-line treatment unless the mutation is very common - like EGFR in non-smokers with lung cancer.
For some, targeted therapy turns cancer into a chronic condition. A stage IV lung cancer patient on osimertinib shared on a cancer forum: “My tumor shrank 80% in eight weeks. I didn’t lose my hair. I didn’t feel like I was dying. I just felt like me.” That’s the promise.
The Future: What’s Next?
The next wave is about timing and teamwork.
Liquid biopsies - blood tests that detect tumor DNA floating in the bloodstream - are now FDA-approved. They can spot resistance mutations months before a scan shows tumor growth. That means doctors can switch drugs earlier, before the cancer spreads further.
AI is stepping in too. IBM Watson for Oncology matched molecular tumor board recommendations in 93% of cases in a 2024 study. It’s not replacing doctors - it’s helping them keep up with the flood of new data.
And researchers are chasing the next frontier: targeting tumor suppressor genes. If we can find a way to restore lost function in TP53, we could help millions. The NCI’s $195 million RESPOND initiative is focused on fixing racial gaps in access - because right now, Black and Hispanic patients are far less likely to get tested or matched with a therapy.
By 2030, experts predict 40% of cancer patients will receive some form of biomarker-driven treatment. But that won’t happen unless testing becomes faster, cheaper, and available to everyone - not just those in big cities with top-tier hospitals.
Final Thoughts
Targeted therapy is not the end of cancer treatment. But it’s the biggest leap forward since chemotherapy. It proves that cancer isn’t one disease - it’s hundreds, defined by DNA, not location. The future belongs to those who can read that code - and act on it quickly, fairly, and affordably.
For patients, it means hope. For doctors, it means responsibility. For the system, it means urgency. We have the tools. Now we need the will to make them work for everyone.
How do I know if targeted therapy is right for me?
You need a tumor biopsy and genomic testing. Ask your oncologist if your cancer type has known actionable mutations - like EGFR, ALK, ROS1, BRAF, or NTRK. If you have advanced cancer, especially lung, melanoma, or colorectal, testing is standard. If you’re unsure, request a referral to a molecular tumor board. They specialize in matching complex genetic results to available treatments.
What if my genetic test comes back with no matches?
About 86% of patients don’t have a match to an approved targeted drug. That doesn’t mean there’s no hope. You may still qualify for a clinical trial testing new drugs. Some mutations are rare but have experimental therapies in development. Talk to your oncologist about enrolling in a trial - many are now open to patients with any cancer type, as long as the genetic target is present.
How long does genetic testing take?
Most commercial tests take 14 to 21 days. Some academic centers can do it faster - around 10 days. If your cancer is progressing quickly, ask about rapid testing options or liquid biopsies, which can sometimes deliver results in 7-10 days. Don’t accept delays without pushing back - time matters.
Are targeted therapies covered by insurance?
Coverage varies. FDA-approved drugs for approved indications are usually covered. But off-label use, rare mutations, or testing costs often get denied. If you’re denied, appeal. Many insurers reverse decisions when you provide clinical trial data or expert opinions. Patient advocacy groups like the Cancer Support Community offer free appeal assistance.
Can targeted therapy cure cancer?
Rarely - but it can control cancer for years. In some cases, like chronic myeloid leukemia with the BCR-ABL mutation, targeted therapy has turned a fatal disease into a manageable condition. For others, it extends life by months or years with better quality. It’s not a cure, but for many, it’s the difference between dying and living.

Kirstin Santiago
January 28, 2026 AT 07:57My mom’s been on osimertinib for 18 months now. She still walks the dog every morning, cooks dinner, and argues with me about Netflix shows. No hair loss, no hospital stays. Just… life. I never thought cancer treatment could feel this normal.
Conor Flannelly
January 30, 2026 AT 00:44It’s wild how we’ve moved from ‘burn it all down’ chemo to precision medicine. Like finally learning the language of the disease instead of yelling at it. 🤔 But I wonder… if we’re treating the map instead of the territory. The tumor’s DNA is just the symptom - what’s really causing the map to glitch?
Conor Murphy
January 30, 2026 AT 20:49My cousin got tested for NTRK after her lung biopsy came back weird. They found the fusion, started her on larotrectinib, and now she’s back teaching art classes. I cried when she sent me a photo of her painting with both hands - no chemo hands, no tremors. Just color. 💙
Marian Gilan
February 1, 2026 AT 03:56They say this is science but it’s all corporate control. Big Pharma invented mutations to sell drugs. Why do you think they stopped funding chemo research? Because pills cost $20k/month and insurance pays. They’re not curing you - they’re renting your body. 🕵️♂️
Desaundrea Morton-Pusey
February 2, 2026 AT 19:53Ugh. Another ‘miracle cure’ post. Meanwhile, my cousin’s insurance denied her test because her cancer was ‘too common.’ They said she should’ve just taken chemo like everyone else. So now she’s in stage 4 and they’re like ‘oops, too late for the magic pill.’
Murphy Game
February 3, 2026 AT 05:08Let’s be real - this is all a numbers game. They test 1000 people, find 138 with a match, then hype up those 138 like they’re the future. Meanwhile, 862 are told ‘sorry, your DNA’s not cool enough.’ This isn’t medicine - it’s genetic elitism.
John O'Brien
February 3, 2026 AT 16:15My oncologist said if I didn’t get tested, I was basically gambling with my life. So I did. Found an ALK fusion. Started on alectinib. Three months later, tumor’s 90% gone. I’m working full time. No nausea. No puking. I’m not ‘lucky’ - I’m just lucky they didn’t treat me like a statistic.
Kegan Powell
February 5, 2026 AT 08:01Genetic testing is like getting the cheat code for your body’s game. But most people don’t even know the game has codes. We need to make this routine - like getting a blood test. No one should have to beg for the right to know what’s inside them. 🤝
Harry Henderson
February 6, 2026 AT 21:05Stop talking about ‘hope’ and start demanding access. If a drug works for NTRK fusion in lung cancer, why is it denied for the same fusion in colon cancer? It’s the same mutation. This isn’t science - it’s bureaucracy with a lab coat. Fight for your right to be treated by your DNA, not your organ.
Kathy McDaniel
February 7, 2026 AT 19:18got my test results back and no matches 😔 but my doc said there’s a trial for my weird mutation and they’ll cover everything. kinda scared but also… kinda hopeful? i’ll go for it. thanks for the post, it helped me ask the right questions.
Paul Taylor
February 8, 2026 AT 14:57Targeted therapy is the future but we’re treating it like a luxury item. It shouldn’t be a privilege of who you are, where you live, or how much insurance you have. We mapped the human genome for $3 billion. Now we’re charging $30k a month to use it? That’s not innovation - that’s exploitation. We need universal genomic access. Period. No more waiting. No more denials. No more ‘it’s not standard for your cancer type.’ It’s standard for your DNA.
April Williams
February 9, 2026 AT 19:28Why do we let Big Pharma decide who lives? They patent mutations like they own them. And then they charge people for the right to live. This isn’t medicine. This is a monopoly. And if you’re poor, Black, or live in a rural town? You’re just supposed to die quietly. I’m done pretending this is fair.