Intermittent Claudication Symptom Tracker
Current Assessment
Mild discomfort that resolves quickly with rest. Usually manageable with lifestyle adjustments.
Noticeable pain that limits activity. May require more frequent breaks and monitoring.
Severe pain or signs of complications (swelling, skin changes). Requires immediate medical attention.
When a pregnant woman experiences intermittent claudication - pain or cramping in the legs caused by reduced blood flow during movement, it can feel unsettling. You might wonder whether it’s safe for your baby, how to stay active, and which treatments are allowed. This guide breaks down what to expect, why pregnancy matters, and practical ways to keep both you and your baby healthy.
Key Takeaways
- Intermittent claudication is a symptom of reduced leg blood flow, not a disease itself.
- Pregnancy raises blood volume and pressure on vessels, which can worsen leg pain.
- Gentle walking, compression stockings, and leg elevation are the safest daily tools.
- Low‑dose aspirin and certain blood‑thinners are sometimes prescribed, but only under a vascular specialist's guidance.
- Seek immediate care if pain appears at rest, your calf swells, or you notice skin colour changes.
What Is Intermittent Claudication?
At its core, intermittent claudication means your leg muscles aren’t getting enough oxygen when you walk or climb stairs. The result is a burning or aching sensation that eases once you stop moving. Most often it signals peripheral arterial disease (PAD), a narrowing of the arteries that deliver blood to the limbs.
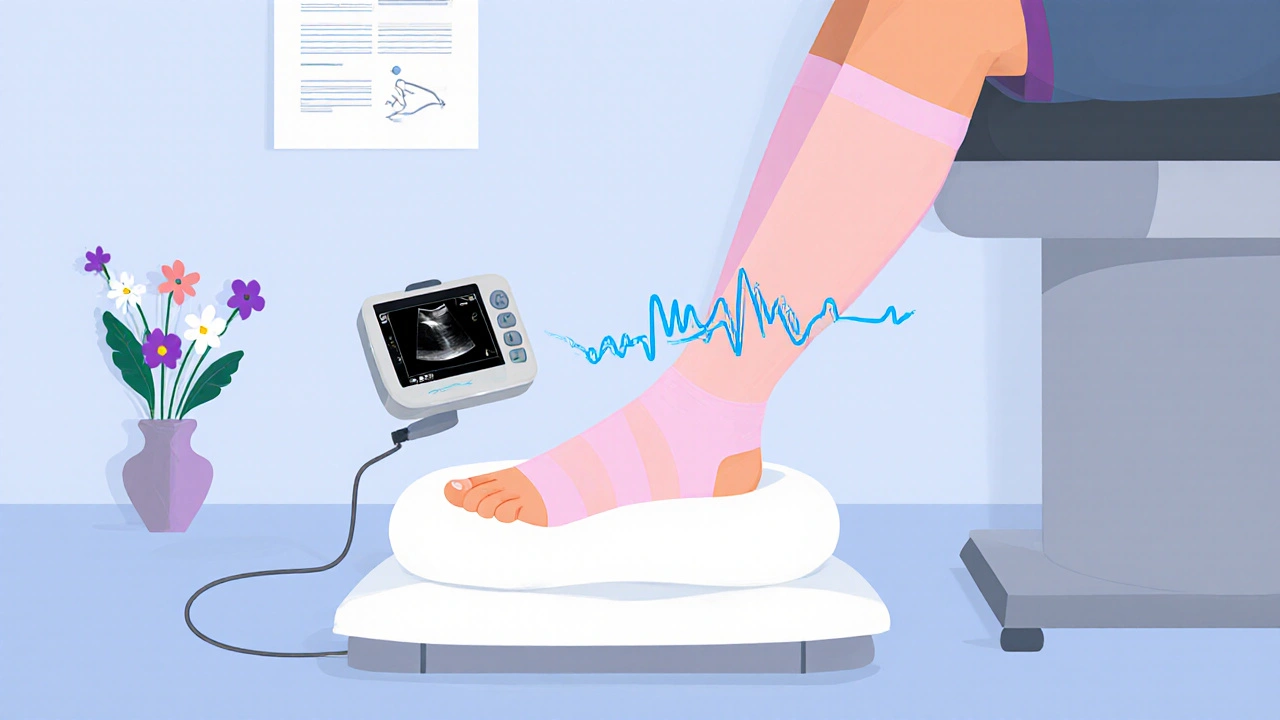
For non‑pregnant adults, doctors usually confirm PAD with a Doppler ultrasound (Doppler test) or an ankle‑brachial index measurement. In pregnancy, those same tools are safe; they use sound waves, not radiation, so the fetus isn’t exposed.
How Pregnancy Changes Blood Flow and Leg Comfort
During pregnancy, your blood volume climbs by about 30‑50%. Hormones also relax vessel walls, and a growing uterus presses on the large veins that return blood from the legs to the heart. This combination can create a bottleneck, making the already narrowed arteries in PAD patients feel tighter.
Some women notice that their usual “walk‑and‑stop” pain appears sooner or lasts longer. The extra weight adds mechanical stress to calf muscles, and swelling (edema) can further compress arteries.
Potential Risks for Mother and Baby
While intermittent claudication itself isn’t usually dangerous for the baby, the underlying PAD can signal broader cardiovascular concerns. Poor circulation may increase the chance of high‑blood‑pressure disorders like pre‑eclampsia. Moreover, if leg pain forces you to stay sedentary, you could gain excess weight and face gestational diabetes.
Rarely, severe PAD can lead to tissue damage (ulcers) if blood flow drops too low. That’s why monitoring symptoms and staying active are essential.
Safe Coping Strategies You Can Start Today
Below are everyday practices that help keep blood moving without risking your pregnancy.
| Strategy | How It Helps | Recommended Frequency |
|---|---|---|
| Gentle walking | Boosts circulation, reduces arterial pressure | 10‑15min, 3‑4times a day |
| Compression stockings | Prevents vein pooling, supports arterial flow | Wear during waking hours |
| Leg elevation | Encourages venous return, eases swelling | 10min after meals or prolonged sitting |
| Water‑based exercise | Low‑impact, improves heart health | 20‑30min, 2‑3times weekly |
| Hydration & balanced diet | Maintains blood viscosity, supports fetal growth | Daily |
Start with short walks around your home or garden. If you feel the pain after a few minutes, pause, elevate your legs, then resume. Over weeks, you’ll likely notice the distance you can walk increases.
Compression stockings should fit snugly but not cut off circulation. Many prenatal clinics stock sizes specifically for pregnant women; ask your midwife for a recommendation.
Leg elevation is simple: prop your feet on a pillow while sitting or lying down. Aim for the heart level to maximize the effect.
Medication Options That Are Pregnancy‑Friendly
Doctors rarely prescribe strong blood‑thinners to pregnant patients because they cross the placenta. However, low‑dose aspirin (81mg) is often considered safe after the first trimester to lower clot risk, especially if you have a history of hypertension.
Statins, the cholesterol‑lowering drugs most people think of for PAD, are contraindicated in pregnancy. Instead, focus on lifestyle changes and, when needed, short courses of calcium channel blockers, but only under a vascular specialist’s supervision.
Always discuss any new supplement, including omega‑3 fatty acids, with your obstetrician to avoid unwanted interactions.

When to Call Your Healthcare Team
If any of these signs appear, reach out immediately:
- Pain at rest or waking you up at night.
- Sudden swelling, especially if one leg looks larger.
- Color change: pale, bluish, or mottled skin on the foot.
- Fever or wound that won’t heal.
- New onset of high blood pressure (>140/90mmHg).
These symptoms could indicate worsening PAD or a separate vascular complication that needs prompt imaging, often a Doppler ultrasound, and possibly a referral to a vascular surgeon.
Putting It All Together: A Sample Daily Plan
- Morning: After breakfast, put on compression stockings and take a 10‑minute gentle walk around the house.
- Mid‑day: If you have a desk job, stand and march in place for 2minutes every hour. Elevate legs for 10minutes after lunch.
- Afternoon: Attend a prenatal water‑aerobics class (if cleared by your doctor). Finish with a short stretch.
- Evening: Light walk after dinner, then sit with feet raised on a pillow while you watch TV.
- Before Bed: Check that stockings are still comfortable, note any new pain, and jot it in a symptom diary to discuss at your next appointment.
This routine balances activity with rest, keeps blood flowing, and gives you clear checkpoints for any concerning changes.
Frequently Asked Questions
Can I continue my regular prenatal vitamins?
Yes. Prenatal vitamins are essential for fetal development and do not interfere with PAD management. Just avoid adding extra iron if your doctor says you’re already iron‑replete.
Is it safe to do yoga while experiencing claudication?
Gentle prenatal yoga is fine, but skip deep forward bends that compress the abdomen. Focus on seated or standing poses that keep blood moving without over‑stretching the calves.
Will my baby be affected if my leg pain worsens?
The pain itself doesn’t harm the baby, but the underlying circulation issue can raise the risk of hypertension, which does affect fetal growth. That’s why monitoring and treatment are important.
Can I wear compression stockings all day?
Generally, yes, as long as they’re properly sized and not too tight. Remove them before bedtime to let skin breathe.
What should I do if I notice a new ulcer on my foot?
Contact your vascular specialist right away. An ulcer can signal critically low blood flow and may need wound care, antibiotics, or a reassessment of your treatment plan.


cris wasala
October 6, 2025 AT 13:57Congrats on noticing the signs and taking steps to track them staying active and listening to your body can make a big difference
Tyler Johnson
October 12, 2025 AT 08:54Understanding intermittent claudication during pregnancy requires a blend of clinical insight and everyday practicality. First, recognize that the growing uterus can compress major blood vessels, leading to reduced perfusion in the lower limbs. This physiological change is normal, yet it can manifest as aching or cramping after prolonged standing. Monitoring the intensity of pain on a scale of one to ten helps differentiate between mild discomfort and a warning sign. It is wise to keep a daily log of activities, noting when symptoms appear and how long they last. Incorporating scheduled rest breaks during the day can prevent the pain from escalating. Simple stretching exercises focusing on the calves and hamstrings promote circulation without overexertion. Hydration also plays a vital role; ample fluid intake supports blood volume and reduces muscle fatigue. Nutrition matters, too, as iron‑rich foods can combat anemia, which sometimes worsens leg pain. If swelling becomes pronounced or skin discoloration is observed, seek medical attention promptly. Remember that each pregnancy is unique, so personal thresholds for pain will vary. Consulting a vascular specialist can provide tailored recommendations for safe exercise. Some clinicians suggest low‑impact activities such as swimming or prenatal yoga to maintain fitness. Wearing supportive footwear with good arch support can lessen strain on the legs. Ultimately, staying informed, listening to your body, and maintaining open communication with your healthcare team will guide you through this challenge safely.
Annie Thompson
October 18, 2025 AT 03:51It's heartbreaking how a condition that should be manageable can feel like a relentless shadow dragging you through each day. The constant ache in the calves becomes a reminder that your body is betraying you at a time when you should be celebrating new life. Even the simplest tasks, like walking to the kitchen, can turn into an arduous trek that leaves you breathless and exhausted. You start to dread the future, wondering if every step will be a struggle, and the optimism that once fluttered within you begins to fade. The medical jargon about perfusion deficits and vascular resistance only adds to the sense of alienation, as if the problem is too complex for simple comfort. While doctors may reassure you with generic advice, the reality is that each flare‑up feels uniquely cruel. You watch other pregnant women glide through their days, oblivious to the silent torment that you endure. The swelling, the tingling, the occasional discoloration - all these signs amplify the feeling of being trapped inside a fragile vessel. Even the recommended rest breaks feel like an admission of weakness, a surrender to an invisible foe. Yet, despite the gloom, there are moments when a gentle massage or a warm compress offers a fleeting glimpse of relief. Those tiny reprieves become treasured islands amid a sea of discomfort. In the end, surviving this ordeal requires a stubborn kind of hope that refuses to be completely snuffed out.
Parth Gohil
October 23, 2025 AT 22:48From a hemodynamic perspective, the gravid uterus exerts extrinsic pressure on the iliac veins, precipitating venous stasis in the distal extremities. This pathophysiological cascade manifests clinically as intermittent claudication, especially during prolonged orthostatic activities. Mitigating strategies include interval walking protocols, ergonomic footgear, and judicious use of compression hosiery to augment venous return. Additionally, integrating low‑impact modalities such as aquatic therapy can preserve cardiovascular conditioning without overloading the vascular compartment. Feel free to reach out if you need a deeper dive into the mechanistic details or personalized regimen tweaks.
VAISHAKH Chandran
October 29, 2025 AT 16:45These guidelines are just watered‑down Western fluff they ignore our true heritage
Pat Merrill
November 4, 2025 AT 11:41Oh wow a tool to track leg pain, because we all have time to become data scientists during pregnancy lol. I guess next they'll ask us to log our cravings in a spreadsheet. But hey, if it gives you peace of mind, go ahead and fill those boxes.
Vicki Roth
November 10, 2025 AT 06:38Noted the importance of regular breaks.
Vishal Bhosale
November 16, 2025 AT 01:35Honestly the tracker looks overcomplicated it could be a simple note app.
Garima Gauttam
November 21, 2025 AT 20:32If we chase metrics we might miss the lived experience of pain and that is where true understanding lies.
Georgia Nightingale
November 27, 2025 AT 15:29Behold the saga of a pregnant woman wrestling with claudication – a drama fit for the ages! While textbooks whisper about vascular compression, real life screams louder with every step. One must orchestrate a symphony of rest, gentle exercise, and vigilant monitoring to keep the plot from turning tragic. Trust me, the climax is far more hopeful when you have a solid care plan.
Chris Kivel
December 3, 2025 AT 10:26Great point staying attuned to your body’s signals is key keep that log handy and share any changes with your doctor early.
sonia sodano
December 9, 2025 AT 05:22Sure, logging every nuance sounds perfect until you realize it adds another layer of stress to an already demanding pregnancy.
Praveen Kumar BK
December 15, 2025 AT 00:19Your description is emotionally heavy but grammatically you missed a comma after “pain” and “especially during prolonged orthostatic activities” could be clearer for readers.
Viji Sulochana
December 20, 2025 AT 19:16Thx for the deep dive love the detail just a quick note the word “orthostatic” is spelt right but you typed “ortho-static” at one point.
Stephen Nelson
December 26, 2025 AT 14:13Ah yes, because dismissing centuries of medical research in favor of nationalist pride is the ultimate solution to claudication.
Fredric Chia
January 1, 2026 AT 09:10While the satirical tone is appreciated, adherence to evidence‑based guidelines remains paramount.
Hope Reader
January 7, 2026 AT 04:07Exactly 😏-a single sentence can sometimes say more than a whole paragraph.
Marry coral
January 12, 2026 AT 23:03You think a simple note app is enough but that’s just lazy and puts moms at risk.
Emer Kirk
January 18, 2026 AT 18:00Metrics can’t capture the weight of every ache.
Roberta Saettone
January 24, 2026 AT 12:57If you need a practical plan beyond the theatrical narrative, consider a structured walking schedule with incremental time increases and regular vascular check‑ups – it works better than drama.