When you're in pain, it's normal to feel frustrated. But when your thoughts spiral into pain catastrophizing, a mental pattern where pain feels overwhelming, uncontrollable, and terrifying. Also known as pain amplification, it turns discomfort into a full-blown crisis in your mind. This isn't weakness—it's a real psychological response that changes how your brain processes pain signals. Studies show people who catastrophize pain report higher pain levels, slower recovery, and more disability—even when the physical injury is the same as someone who doesn't.
This pattern doesn't happen in isolation. It’s closely tied to chronic pain, persistent discomfort that lasts beyond normal healing time, like fibromyalgia or long-term back issues. When pain sticks around, your brain can start expecting it, fearing it, and even predicting it before it happens. That’s where psychological pain, the emotional and mental burden that comes with physical discomfort takes over. It’s not "all in your head"—it’s your head actually making the pain worse. You might find yourself avoiding movement, obsessing over symptoms, or feeling hopeless about improvement. These thoughts don’t just make you feel bad—they slow healing, reduce the effectiveness of meds, and increase reliance on opioids.
What’s surprising is how often this shows up in conditions you wouldn’t expect. People with pain catastrophizing are more likely to struggle with side effects from medications like SSRIs or NSAIDs, especially when those drugs are used for long-term pain. They’re also more prone to rebound effects, like nasal congestion from overused sprays, because stress and fear make the body hypersensitive. Even something as simple as diet during chemotherapy can feel impossible when your mind is stuck in a loop of "this will never get better."
Pain catastrophizing doesn’t mean you’re exaggerating. It means your nervous system is stuck on high alert. The good news? It can be rewired. Cognitive behavioral techniques, mindfulness, and even gentle movement have been shown to reduce this pattern. You’re not alone—thousands of people with chronic conditions like fibromyalgia, pancreatitis, or arthritis deal with this every day. Below, you’ll find real, practical guides on how pain connects to medications, lifestyle, and mental health. These aren’t theoretical—they’re from people who’ve been there and found ways to break the cycle.
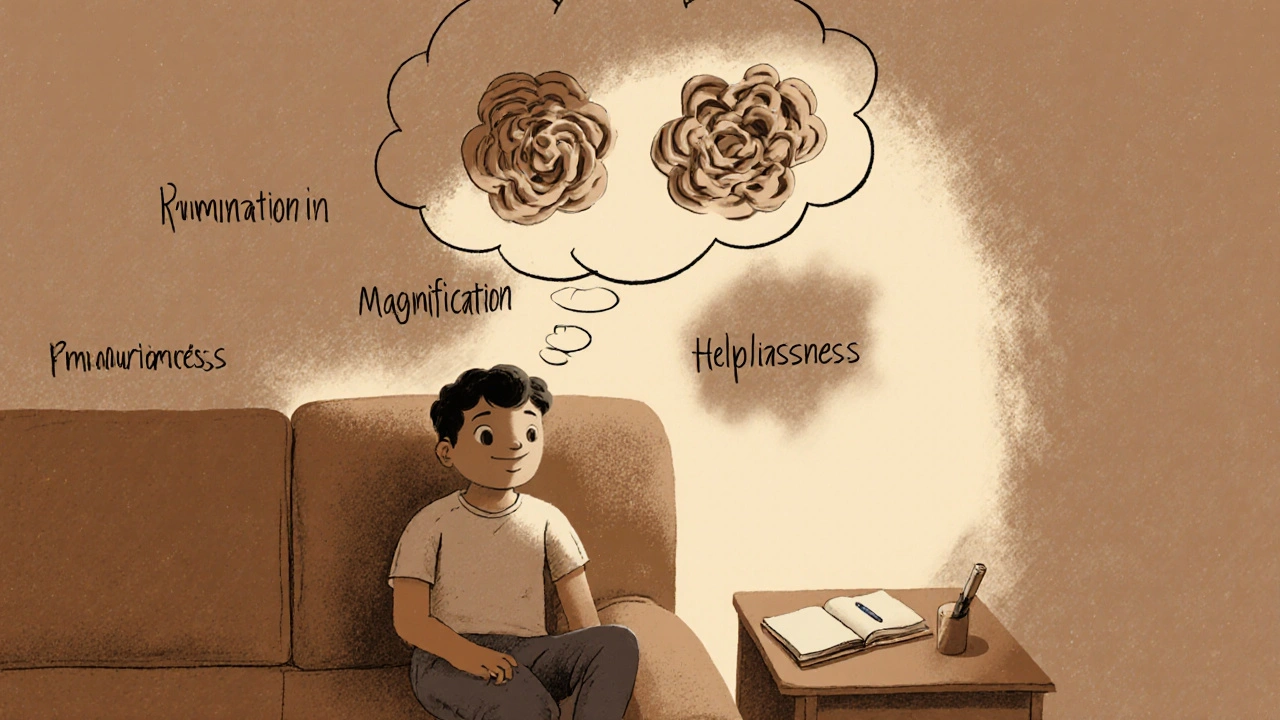
Pain catastrophizing makes pain feel worse by amplifying fear and helplessness. CBT offers practical tools to break the cycle by identifying distorted thoughts, challenging them, and slowly rebuilding confidence in movement and daily life.
Nov 17 2025
Menu