When your back flares up and your mind immediately goes to "This is never going to end," "I’ll never be able to work again," "What if I’m stuck like this forever?" - you’re not just feeling pain. You’re caught in pain catastrophizing.
This isn’t just "being negative." It’s a real psychological pattern that makes pain feel worse, last longer, and take over your life. Research shows it’s one of the strongest predictors of poor outcomes in chronic pain - stronger than the actual physical damage. The good news? You can change it. Cognitive Behavioral Therapy (CBT) isn’t just talk. It’s a set of proven tools that help you untangle the knot between your thoughts and your pain.
What Exactly Is Pain Catastrophizing?
Pain catastrophizing happens when your brain turns pain into a disaster. It’s not about being weak or dramatic. It’s a pattern of thinking with three clear parts:
- Rumination: You can’t stop thinking about the pain. It loops in your head like a broken record.
- Magnification: You believe the pain means something terrible is happening - "This ache is a sign of something serious," or "If it hurts this much, I must be damaging myself."
- Helplessness: You feel like there’s nothing you can do. No matter what you try, the pain wins.
This isn’t just in your head - it’s in your nervous system. Brain scans show that when you catastrophize, areas linked to emotion and threat detection light up more. That means your brain is actually amplifying the pain signal. A 2024 study in Nature Scientific Reports found that CBT helps separate these two things: the physical sensation of pain, and the catastrophic thoughts about it. When they’re untangled, pain becomes less overwhelming.
How Do You Know If You’re Catastrophizing?
The Pain Catastrophizing Scale (PCS) is the standard tool used by clinicians. It’s 13 simple questions rated from 0 to 4. A score of 30 or higher means you’re in the clinically significant range. But you don’t need a test to spot it.
Ask yourself:
- Do I immediately assume the worst when I feel pain?
- Do I replay painful moments over and over in my mind?
- Do I feel like I have no control, no matter what I do?
- Do I avoid activities because I’m afraid the pain will get worse?
If you answer yes to most of these, you’re likely caught in the cycle. And you’re not alone. In VA clinics, nearly 40% of chronic pain patients score above 30 on the PCS. In community settings, it’s about 25%. The good news? CBT works - especially when it’s targeted.
How CBT Breaks the Cycle
CBT doesn’t tell you to "think positive." It teaches you to notice, question, and redirect your thoughts. Here’s how it actually works in practice:
1. Self-Monitoring: Catch the Thought Before It Spirals
The first step is awareness. You start keeping a simple log:
- Trigger: What happened right before the pain spiked? (e.g., standing up, walking the dog, hearing a loud noise)
- Thought: What ran through your mind? (e.g., "This is going to ruin my whole week")
- Feeling: What emotion came up? (fear, dread, panic)
- Behavior: What did you do? (stopped moving, called in sick, canceled plans)
- Pain Level: On a scale of 1-10, how bad was it?
After a few days, patterns emerge. You start seeing that it’s not the activity that makes pain worse - it’s the thought about the activity. A 45-year-old woman with fibromyalgia reduced her PCS score from 42 to 18 in 12 weeks using this method. Her pain intensity dropped by half. She went back to part-time work.
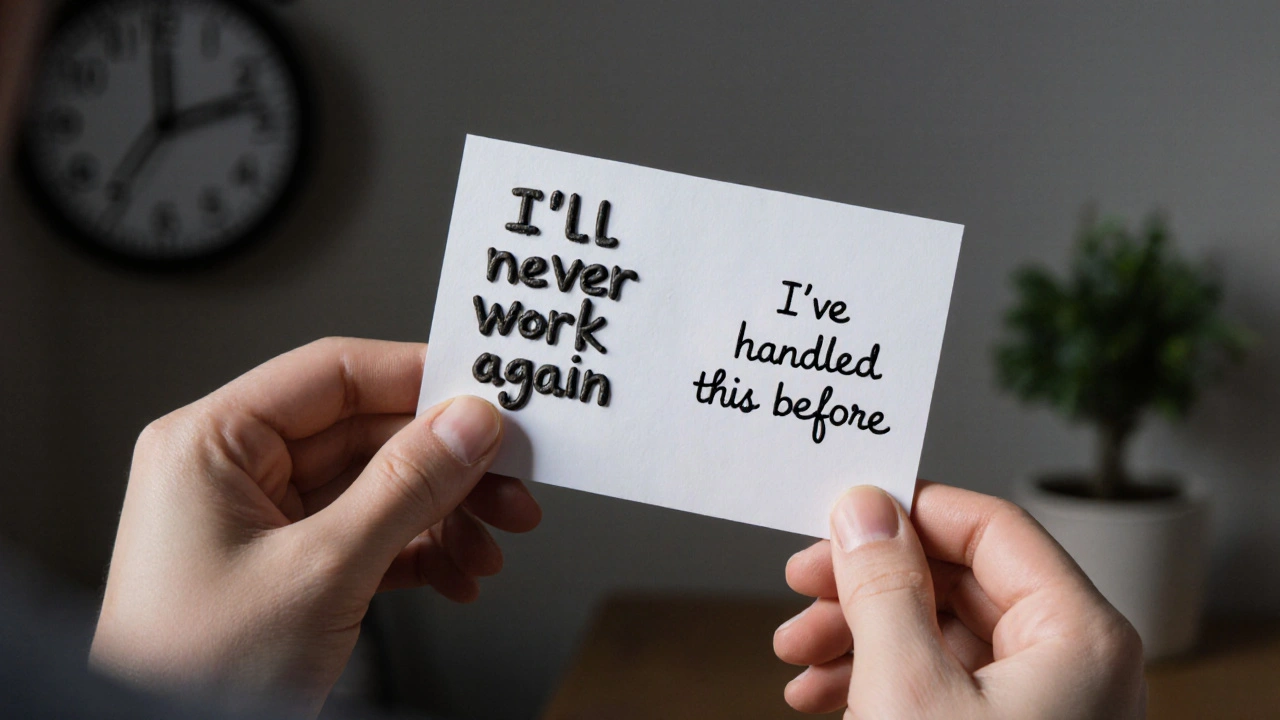
2. Cognitive Restructuring: Challenge the Story
Once you spot a catastrophic thought, you don’t fight it. You question it. Think of it like being a detective in your own mind.
Take this thought: "If I walk for 10 minutes, I’ll be in bed for three days."
- Is this fact or fear? Have you actually been in bed for three days after walking 10 minutes before?
- What’s the evidence? What’s the worst that actually happened last time?
- What’s a more realistic thought? "Walking 10 minutes might make me sore, but I’ve done it before and recovered. I can rest if I need to."
This isn’t about lying to yourself. It’s about replacing the worst-case script with a more accurate one. The VA’s Whole Health Library calls this "unhooking" from negative thinking. It’s not magic - it’s practice.
3. Behavioral Activation: Move Even When It’s Hard
Catastrophizing leads to avoidance. Avoidance leads to stiffness, weakness, and more pain. CBT flips this by gently pushing you back into movement - not to "fix" the pain, but to prove to your brain that you’re not helpless.
Start small. Walk for 5 minutes. Do 3 stretches. Wash one dish. Then track what happened. Did the pain get worse? Did you collapse? Or did you feel a little tired, but okay? Over time, your brain learns: "Walking doesn’t mean disaster. I can handle this."
One study showed that combining CBT with light exercise had the strongest effect - reducing catastrophizing scores by 1.0 standard deviation compared to no treatment. That’s bigger than most medications.
What Works Better Than CBT?
Nothing - for pain catastrophizing specifically.
A 2023 review by the International Association for the Study of Pain looked at dozens of studies. When researchers focused only on people with high levels of catastrophizing, CBT was the only treatment that showed a strong, reliable effect. Acceptance and Commitment Therapy (ACT) helped, but not as much. Medications? They might reduce pain, but they don’t touch the thought patterns driving the distress.
And here’s the kicker: CBT doesn’t just help with pain. It helps with anxiety, depression, and sleep - all of which get worse when you’re stuck in a catastrophizing loop.
What Gets in the Way?
CBT isn’t a quick fix. It takes time. Most people need 8 to 12 weeks of weekly sessions to see real change. And it’s hard - especially when your pain is high.
One Reddit user wrote: "When my pain is at an 8/10, I just don’t have the mental energy to do CBT exercises." That’s real. When your body is screaming, your brain is in survival mode. Trying to analyze thoughts feels impossible.
That’s why many people drop out. About 22% of patients quit before they see results. The key? Start small. Use apps. Try a 5-minute daily reflection instead of a full journal. Use voice notes if writing feels too much. Progress isn’t linear. Some days you’ll feel stuck. That’s normal.
Also, CBT works best when you’re not dealing with severe depression or trauma. If you’re in crisis, those issues need to be addressed first. CBT is powerful - but not a magic bullet for every pain problem.

Tools You Can Use Today
You don’t need a therapist to start. Here are three practical tools you can use right now:
- The 3-Question Check: When pain spikes, ask: Is this thought based on facts or fear? What’s the evidence? What’s a more balanced thought?
- Thought Replacement Cards: Write down your top 3 catastrophic thoughts on index cards. On the back, write a realistic, calm response. Keep them in your wallet or phone case.
- Micro-Movement: Pick one activity you’ve avoided because of pain. Do it for 2 minutes today. Just 2 minutes. Then write down what happened - not how you felt, but what actually occurred.
Apps like Curable and PainScale have CBT-based modules built in. Over 450,000 people are using them. They’re not perfect, but they’re accessible - and they work.
What’s Next for Pain Catastrophizing Treatment?
The future is getting smarter. The VA is rolling out a digital Pain Management Dashboard across all its centers by the end of 2024. It tracks your PCS scores over time and gives real-time feedback. Stanford is testing smartphone alerts that pop up when you’re likely catastrophizing - like when you’re lying awake at 3 a.m. - and guide you through a 90-second CBT exercise.
By 2025, 75% of pain clinics in the U.S. will screen for catastrophizing. That’s up from 62% just five years ago. This isn’t a trend. It’s a shift in how we treat pain - from just numbing the body to healing the mind too.
Final Thought
Pain catastrophizing isn’t your fault. It’s a brain habit - one that developed because your nervous system was trying to protect you. But now, it’s hurting you more than helping.
CBT doesn’t promise you’ll never feel pain again. It promises you’ll stop letting pain control your thoughts, your choices, and your life. You don’t have to believe the worst. You just have to learn to question it. And that’s something you can start today - one thought, one breath, one small movement at a time.

Emily Entwistle
November 19, 2025 AT 01:42Duncan Prowel
November 20, 2025 AT 06:11Bruce Bain
November 21, 2025 AT 03:01Jonathan Gabriel
November 22, 2025 AT 03:56Don Angel
November 23, 2025 AT 08:24benedict nwokedi
November 24, 2025 AT 09:18malik recoba
November 24, 2025 AT 17:02Sarbjit Singh
November 25, 2025 AT 21:49Angela J
November 26, 2025 AT 06:42Sameer Tawde
November 27, 2025 AT 13:55Jeff Hakojarvi
November 28, 2025 AT 14:42Timothy Uchechukwu
November 30, 2025 AT 12:26Ancel Fortuin
December 1, 2025 AT 13:28Hannah Blower
December 2, 2025 AT 13:37