When you hear teplizumab, a monoclonal antibody approved to delay the onset of type 1 diabetes in high-risk individuals. It's not a cure, but it’s the first drug that can actually slow down the immune system’s attack on insulin-producing cells. This isn’t just another diabetes pill—it’s a targeted immune therapy designed to stop the disease before it fully takes hold.
Teplizumab works by binding to a specific protein on T-cells, the immune cells that mistakenly destroy the pancreas in type 1 diabetes. Think of it like putting a brake on the body’s own attack system. It doesn’t suppress the whole immune system like steroids do. Instead, it quietly redirects just the harmful cells. This precision is why it’s used in people with stage 2 type 1 diabetes—those who still make some insulin but have multiple autoantibodies showing the disease is coming. The FDA approved it after a landmark study showed it could delay full-blown diabetes by an average of three years. That’s not just a delay—it’s time to plan, adjust, and maybe even avoid insulin injections for longer.
Teplizumab is part of a bigger shift in how we treat autoimmune diseases. It’s not alone. Drugs like insulin glargine, a long-acting insulin used to manage blood sugar in type 1 and type 2 diabetes, help control symptoms, but teplizumab tries to fix the root cause. It’s also related to other immunotherapy, a class of treatments that train or modulate the immune system to fight disease approaches being tested for lupus, multiple sclerosis, and even type 2 diabetes. What’s clear is that medicine is moving from managing symptoms to stopping disease progression—and teplizumab is leading that charge in diabetes.
You won’t find teplizumab in a pill bottle. It’s given as a daily IV infusion over 14 days, usually in a clinic. Side effects include temporary drops in white blood cells, rashes, and headaches. It’s not for everyone. But for families with a history of type 1 diabetes, or kids testing positive for multiple autoantibodies, it’s a real game-changer. The science behind it is solid, and the results are measurable. What’s next? More trials, better timing, and maybe even combinations with other drugs to make the effect last longer.
Below, you’ll find articles that dig into how drugs like teplizumab fit into the bigger picture of diabetes care, immune system triggers, and how treatments like dexamethasone, SSRIs, and insulin glargine interact with the body in different ways. Whether you’re a patient, caregiver, or just curious, these posts give you the real facts—not the hype.
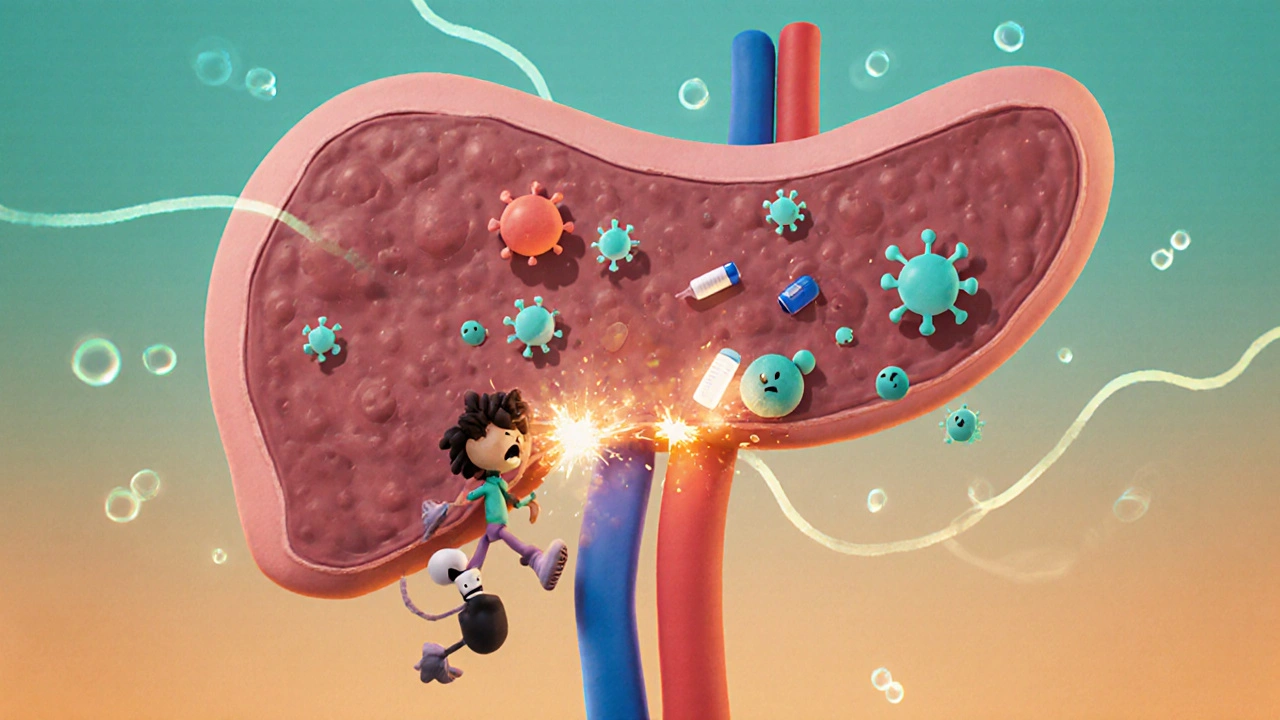
Type 1 diabetes is an autoimmune disease that destroys insulin-producing cells in the pancreas. Learn how it develops, why insulin is essential, and what new treatments like teplizumab and stem cell therapy are changing the future of management.
Nov 13 2025
Menu