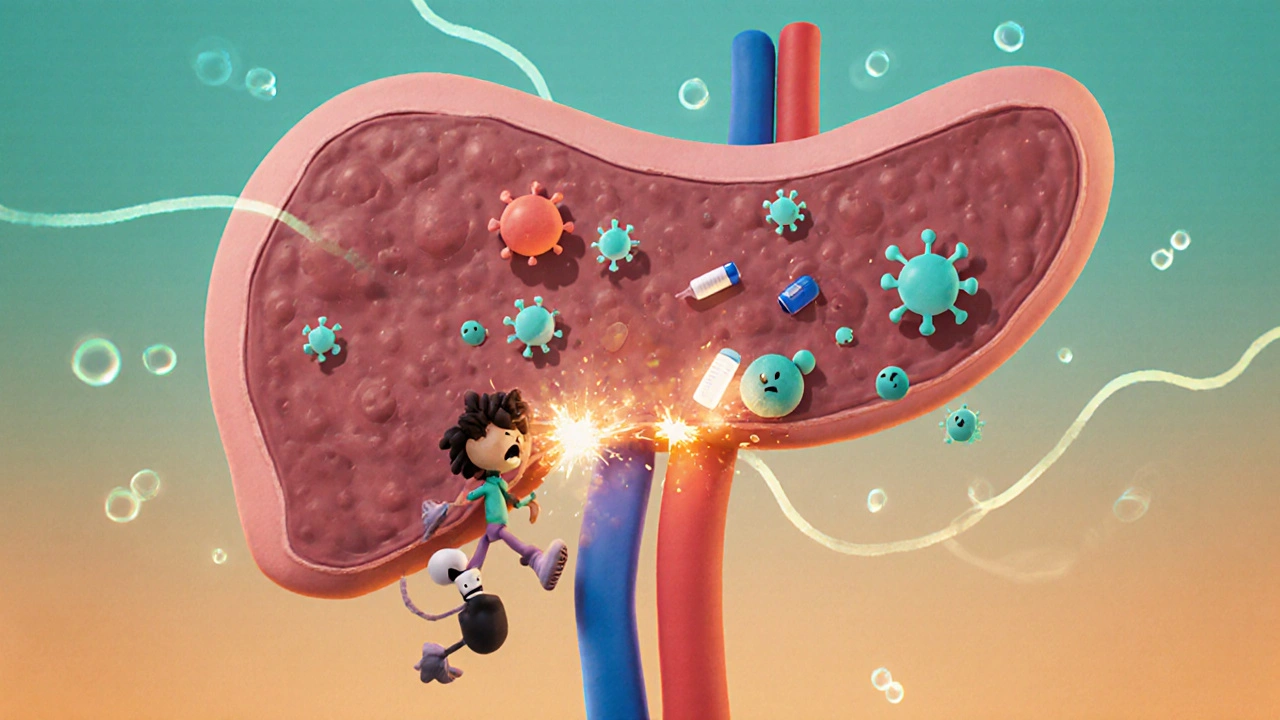
Type 1 diabetes isn’t just about high blood sugar. It’s the result of your immune system turning against your own pancreas-specifically, the insulin-making beta cells. This isn’t a lifestyle issue. It’s not caused by eating too much sugar. It’s an autoimmune disease where your body’s defense system mistakes healthy cells for invaders and destroys them. Once those beta cells are gone, your body can’t make insulin anymore. And without insulin, glucose can’t enter your cells to be used for energy. That’s why people with type 1 diabetes need insulin every single day-just to survive.
How the Immune System Attacks the Pancreas
The process starts long before symptoms appear. Years before someone is diagnosed, their immune system begins targeting proteins inside the insulin-producing beta cells. These proteins-like insulin itself, GAD65, IA-2, and ZnT8-become targets for autoantibodies. These antibodies don’t cause damage directly, but they’re a red flag that the immune attack is underway. The real destruction comes from T-cells, which invade the pancreas in a process called insulitis. These immune cells literally eat away at the beta cells until there’s not enough left to produce insulin.
Genetics play a big role. If you carry the HLA-DR3 or HLA-DR4 gene variants, your risk jumps 20 to 30 times higher than average. But genes alone don’t cause it. Something has to trigger the attack. Viruses, especially coxsackievirus B, are strong suspects. Studies show people who had detectable viral RNA in their blood months before diagnosis were 58% more likely to develop type 1 diabetes. Other triggers might include early diet, gut bacteria imbalances, or even stress-but the exact recipe varies from person to person.
Three Stages Before Diagnosis
Type 1 diabetes doesn’t show up overnight. Experts now define it in three clear stages:
- Stage 1: You have two or more autoantibodies, but your blood sugar is still normal. You don’t feel sick. This stage affects about 0.4% of the general population.
- Stage 2: Your blood sugar is starting to rise, but you still don’t have symptoms. Your body is struggling to make enough insulin. About 0.15% of people are in this stage.
- Stage 3: Symptoms hit-excessive thirst, frequent urination, unexplained weight loss, fatigue. At this point, you’ve lost most of your beta cells and need insulin immediately.
This staging system changes everything. It means we can now identify people at risk before they get sick. That’s where new treatments like teplizumab come in. Approved by the FDA in 2022, teplizumab is the first drug that can delay the onset of stage 3 type 1 diabetes. In clinical trials, it pushed back diagnosis by nearly two and a half years on average. It doesn’t cure the disease, but it buys time-time to prepare, learn, and adjust.
Insulin Isn’t Optional-It’s Life-Saving
Once your body stops making insulin, there’s no workaround. You must replace it. That means either multiple daily injections or an insulin pump. Most people use rapid-acting insulin (like aspart or lispro) before meals and long-acting insulin (like glargine or degludec) for background coverage. The starting dose? Around 0.5 units per kilogram of body weight per day, split evenly between basal and bolus.
But insulin dosing isn’t guesswork anymore. Continuous glucose monitors (CGMs) like the Dexcom G7 give real-time readings every five minutes. These devices have cut hypoglycemic episodes by 40-50% and lowered HbA1c by 0.4-0.6% on average. Even better are closed-loop systems-also called artificial pancreases. Devices like Tandem’s Control-IQ automatically adjust insulin delivery based on your glucose trends. People using them spend 71-74% of the day in the target range (70-180 mg/dL), compared to just 51-55% with traditional pumps.
Why Some People Are Misdiagnosed
One in eight adults newly diagnosed with type 1 diabetes is initially told they have type 2. Why? Because they’re older. Because they’re not thin. Because doctors assume insulin resistance is the cause. But the truth is, adults can develop type 1 diabetes too. This is called LADA-Latent Autoimmune Diabetes in Adults. It progresses slower than childhood-onset type 1, so people may stay off insulin for years. But without proper diagnosis, they’re given the wrong meds-like metformin-which do nothing to stop the immune attack.
Testing for autoantibodies and measuring C-peptide levels (a marker of your body’s own insulin production) can clear this up. People with type 1 diabetes have C-peptide levels below 0.2 nmol/L at diagnosis. Those with type 2 usually stay above 0.6 nmol/L. If you’re an adult diagnosed with type 2 but aren’t responding to oral meds, ask for these tests.
The Rare Link to Autoimmune Pancreatitis
Most people with type 1 diabetes have no issues with their exocrine pancreas-the part that makes digestive enzymes. But in about 1 in 300 cases, the autoimmune attack spills over. This is called autoimmune pancreatitis (AIP). It causes inflammation in the ducts and tissue of the pancreas, leading to abdominal pain, bloating, and malabsorption.
AIP comes in two types. Type 1 is linked to high IgG4 levels and responds well to steroids. Type 2 is tied to inflammatory bowel disease. When AIP happens alongside type 1 diabetes, treatment gets complex. Steroids help the pancreas, but they also spike blood sugar. So insulin doses often need to go up dramatically during treatment. These patients need both an endocrinologist and a gastroenterologist working together. The American Diabetes Association now recommends checking for pancreatic enzyme deficiencies in anyone with type 1 who has ongoing digestive problems.

What’s Next? Emerging Therapies
Science is moving fast. Teplizumab was just the beginning. Right now, over 15 clinical trials are testing new ways to stop or reverse type 1 diabetes. One drug, abatacept, slowed beta-cell loss by 59% over two years in early-stage patients. Another, verapamil-a common blood pressure pill-showed it could preserve 30% more insulin production in newly diagnosed adults.
The most exciting breakthrough? Stem cell-derived islet cell transplants. Vertex Pharmaceuticals’ VX-880 therapy took 12 people with severe type 1 diabetes and gave them lab-grown beta cells. At 90 days, 89% were producing their own insulin again. One patient stopped using insulin entirely. These aren’t cures yet-patients still need immunosuppressants-but they’re proof that replacing lost cells is possible.
And then there’s the gut. Researchers found that 67% of people with type 1 diabetes have less of a specific gut bacteria called Faecalibacterium prausnitzii. This bug produces butyrate, which helps calm inflammation. Studies are now testing probiotics and fiber-rich diets to see if fixing the gut can slow the autoimmune attack.
Living Well With Type 1 Diabetes
Managing type 1 diabetes isn’t about perfection. It’s about consistency. Check your glucose. Take your insulin. Count your carbs. Adjust for activity. Sleep well. Manage stress. These aren’t just tips-they’re survival tools.
And you’re not alone. In the U.S., 1.25 million people live with type 1 diabetes. Worldwide, it’s 8.7 million. The cost? Nearly $20,000 per person per year, with insulin alone making up a third of that. But new technologies, better access to care, and smarter treatments are making life easier than ever.
If you or someone you know has type 1 diabetes, remember: this disease is not your fault. It’s not a failure of willpower. It’s a medical condition with a biological cause. And with the right tools and support, you can live a full, active, healthy life.
Is type 1 diabetes the same as autoimmune pancreatitis?
No. Type 1 diabetes attacks the insulin-producing beta cells in the endocrine pancreas. Autoimmune pancreatitis attacks the exocrine pancreas-the part that makes digestive enzymes. They’re separate conditions, but in rare cases (about 1 in 300), both happen together. When they do, it’s called a broader autoimmune pancreatic syndrome and requires coordinated care from both an endocrinologist and a gastroenterologist.
Can type 1 diabetes be cured?
Not yet, but we’re getting closer. There’s no cure today, but new therapies like teplizumab can delay diagnosis by years. Stem cell transplants have restored insulin production in some patients, and some have even stopped needing insulin. These are early results, but they prove the body can be restored. Research is accelerating, and the goal is no longer just managing blood sugar-it’s stopping the immune attack and replacing lost cells.
Why do some people with type 1 diabetes still make a little insulin?
Even after diagnosis, many people still have a small number of surviving beta cells. These cells can produce tiny amounts of insulin, measured as C-peptide. People with higher C-peptide levels have fewer blood sugar swings and lower risk of complications. This is why treatments that protect these remaining cells-like verapamil or teplizumab-are so important. The goal isn’t just to add insulin; it’s to preserve what’s left.
Can diet or fasting reverse type 1 diabetes?
No. Diet and fasting can’t bring back destroyed beta cells or stop the autoimmune attack. While a healthy diet helps manage blood sugar and reduces complications, it cannot replace insulin. Some people claim to have reversed type 1 diabetes after extreme diets, but these are either misdiagnosed cases (likely LADA or type 2) or temporary improvements due to weight loss or reduced carb intake. Insulin remains essential for survival.
How do I know if I have LADA and not type 2 diabetes?
If you’re an adult diagnosed with type 2 but aren’t responding to metformin or other oral meds, ask for autoantibody testing (GAD65, IA-2) and a C-peptide test. LADA patients typically have positive autoantibodies and low C-peptide levels, even if they’re not yet on insulin. Many are misdiagnosed because they’re older and not underweight. LADA is still type 1 diabetes-it just progresses slower.
Is teplizumab available for everyone with type 1 diabetes?
No. Teplizumab is only approved for people in Stage 2-those with two or more autoantibodies and abnormal blood sugar but no symptoms yet. It’s not for people already on insulin (Stage 3). It’s also not for children under 8. Screening for autoantibodies is key. If you have a close relative with type 1 diabetes, you may be eligible for free screening through TrialNet.

Brian Bell
November 13, 2025 AT 04:35Eleanora Keene
November 13, 2025 AT 05:07Ryan Anderson
November 14, 2025 AT 01:25gent wood
November 15, 2025 AT 04:05Peter Aultman
November 17, 2025 AT 00:51Brittany C
November 18, 2025 AT 17:22Anjan Patel
November 20, 2025 AT 04:01Sean Evans
November 20, 2025 AT 10:37Hrudananda Rath
November 21, 2025 AT 16:00Kevin Wagner
November 22, 2025 AT 06:19Don Ablett
November 22, 2025 AT 11:54kshitij pandey
November 22, 2025 AT 17:20Joe Goodrow
November 23, 2025 AT 14:55