Nonalcoholic fatty liver disease isn’t just about being overweight. It’s a silent, growing threat affecting 1 in 4 people worldwide-and nearly 100 million Americans. Once called NAFLD, it’s now officially known as MASLD (metabolic dysfunction-associated steatotic liver disease), a name that better reflects what’s really going on: your liver is drowning in fat because your metabolism is out of balance. And here’s the scary part-you might not feel a thing until it’s too late.
What Exactly Is MASLD?
MASLD means your liver has more than 5% fat in its cells-not because you drink alcohol, but because your body can’t process sugar and fat properly. This isn’t a rare condition anymore. It’s the most common liver disease on the planet. In the U.S., it’s linked to obesity, type 2 diabetes, high blood pressure, and high triglycerides. These aren’t just separate health issues-they’re all pieces of the same puzzle called metabolic syndrome.
At first, it’s just fat buildup (steatosis). That’s stage one. But if nothing changes, inflammation kicks in. That’s when it becomes MASH (metabolic dysfunction-associated steatohepatitis), the more serious form. From there, scarring can start. And once scar tissue builds up, your liver can’t heal itself. That’s fibrosis. Then cirrhosis. Then, in some cases, liver cancer.
The good news? In the early stages, MASLD is completely reversible. The bad news? Most people don’t know they have it until their liver enzymes show up high on a routine blood test-or worse, until they’re already in advanced disease.
Who’s at Risk?
You don’t have to be obese to get MASLD, but it’s a huge red flag. About 70% of people with type 2 diabetes have it. Up to 90% of those with severe obesity do. But here’s what most people miss: you can have normal weight and still have MASLD. That’s called "lean MASLD." It’s less common, but it happens-especially in people with insulin resistance or a family history of liver disease.
Some groups are hit harder:
- Hispanic populations have the highest rates-nearly 45%
- Non-Hispanic Black individuals have lower rates, around 20%
- Non-Hispanic whites sit at about 24%
And it’s not just adults. Kids are getting it too. One in ten children now has fatty liver disease. In obese kids? That jumps to 7 out of 10. Pediatricians are seeing it in 10-year-olds. This isn’t a future problem-it’s happening right now.
Why It’s So Hard to Diagnose
MASLD doesn’t scream for attention. Most people have no symptoms. A few might feel tired or have mild discomfort under the right rib cage. But those signs are easy to brush off as stress, aging, or just "feeling off."
Doctors used to rely on liver enzyme tests-ALT and AST. But here’s the catch: 30% of people with advanced MASLD have normal liver enzymes. So if your blood test looks fine, that doesn’t mean your liver is healthy.
The gold standard for diagnosis used to be a liver biopsy. But that’s invasive, expensive, and carries small risks. Now, non-invasive tools are catching up. FibroScan (a special ultrasound that measures liver stiffness) and blood tests like the ELF panel are becoming more common. Still, insurance often won’t cover them unless you’re already in advanced stages.
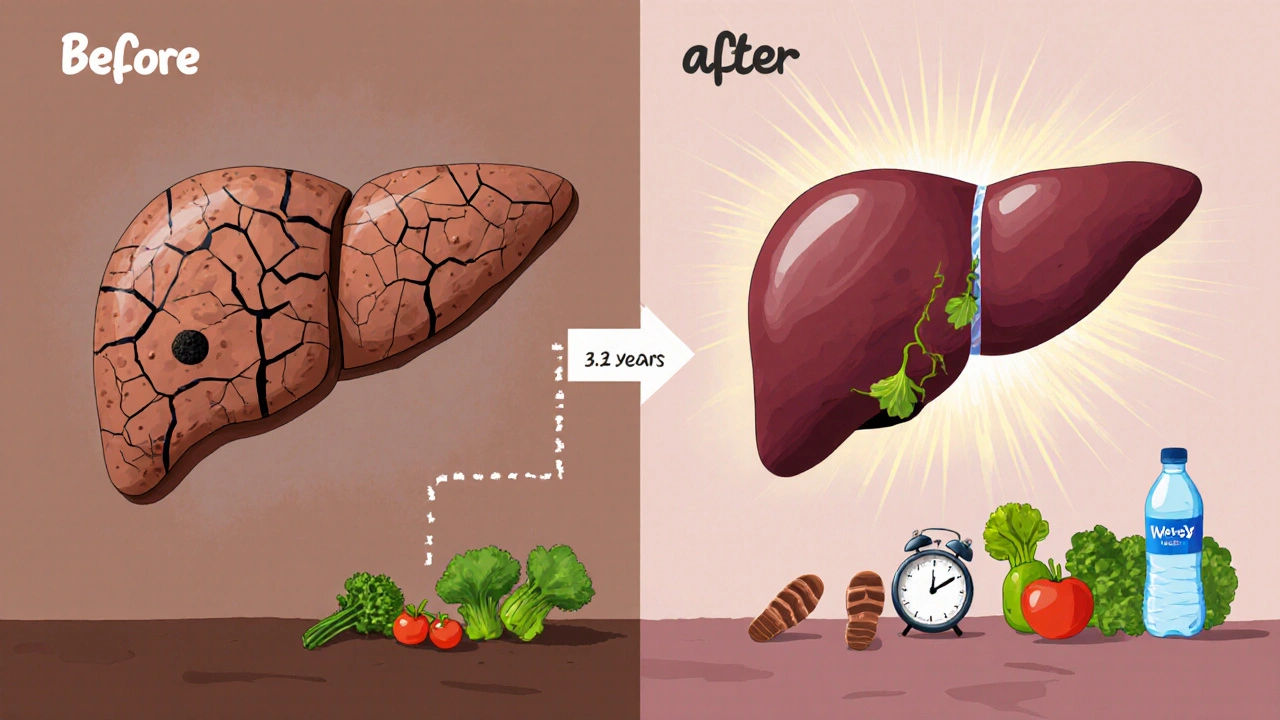
Patients report waiting an average of 3.2 years to get a proper diagnosis. Many are told their elevated liver enzymes are "benign"-a term that’s dangerously misleading.

What Makes MASLD Worse?
It’s not just sugar and fat. It’s how they interact with your body.
Insulin resistance is the engine behind MASLD. When your cells stop responding to insulin, your liver gets flooded with glucose. It turns that glucose into fat-and stores it right in the liver. This process also triggers inflammation.
Processed carbs (white bread, sugary drinks, pastries) spike blood sugar fast. That’s a direct signal to your liver: "Make more fat." Even "healthy" foods like fruit juice can be problematic if you’re drinking them daily.
Lack of movement is another big one. Sitting for long periods slows down fat metabolism. Even if you exercise on weekends, if you’re sedentary the rest of the week, your liver still suffers.
Genetics play a role too. A gene variant called PNPLA3 is linked to higher fat storage in the liver, especially in Hispanic populations. But genes aren’t destiny. Lifestyle still controls whether those genes get activated.
How to Prevent and Reverse MASLD
There’s no pill for MASLD. Not yet. The FDA approved resmetirom in March 2024-the first drug for MASH-but it’s only for advanced cases. Prevention and early reversal? That’s all lifestyle.
Here’s what actually works, backed by clinical data:
- Loose 5-7% of your body weight. That’s not "get skinny." That’s 10-15 pounds for most people. Studies show this cuts liver fat by 30% and reverses steatosis in 81% of cases.
- Go for 10,000 steps a day. Walking isn’t just cardio-it’s a metabolic reset. It improves insulin sensitivity without needing a gym membership.
- Adopt the Mediterranean diet. Focus on vegetables, beans, fish, olive oil, nuts, and whole grains. Cut out added sugar, fried foods, and ultra-processed snacks. People who stick with this diet for 6 months see a 76% improvement in liver fat.
- Avoid alcohol. Even small amounts can make MASLD worse. The American Association for the Study of Liver Diseases recommends zero alcohol.
- Get tested if you’re at risk. If you have diabetes, obesity, high blood pressure, or high triglycerides, ask your doctor for a FibroScan or liver enzyme panel. Don’t wait for symptoms.
Real people are reversing this. One Reddit user, u/HealthyLiverJourney, dropped 8% of their body weight over a year with daily walks and diet changes. Their FibroScan score went from 9.8 kPa (moderate scarring) to 5.2 kPa (normal). That’s not luck-that’s consistency.
Why Most People Fail
People don’t fail because they’re lazy. They fail because the advice is too vague. "Eat better and exercise more" doesn’t cut it.
Here’s what actually helps:
- Track your meals for two weeks-not to count calories, but to spot patterns. Are you drinking soda? Snacking after dinner? Eating out three times a week?
- Start small. Swap one sugary drink for water. Take a 15-minute walk after dinner. Do 10 squats while brushing your teeth.
- Build habits, not goals. Don’t say, "I want to lose 20 pounds." Say, "I’m going to walk every day for the next 30 days."
- Find support. Online communities like LiverLife or r/NAFLD help people stay accountable. 76% of users who joined these groups stuck with their plan.
Most people quit exercise programs within 3 months-not because they don’t care, but because they’re tired, sore, or discouraged. That’s why daily movement matters more than intense workouts.
What’s Changing in 2025?
The landscape is shifting fast. In 2025, non-invasive blood tests will become widely available to detect advanced fibrosis with 89% accuracy. That means you might not need a biopsy anymore.
Workplaces are stepping in too. Companies like IBM have cut NAFLD rates among employees by 37% in three years by offering free nutrition coaching, gym access, and metabolic health screenings.
And research is moving fast. New drugs are in phase 3 trials. But none of them will work if you don’t fix the root cause: your metabolism.
The Bottom Line
MASLD isn’t a liver problem. It’s a whole-body problem. Your liver is just the warning light.
You can stop it. You can reverse it. But only if you act before the damage becomes permanent. The window is wide open-for now. Once fibrosis sets in, it’s much harder to turn back.
Start today. Walk. Eat real food. Cut out sugar. Get tested. Don’t wait for a diagnosis. If you have metabolic risk factors, you’re already at risk. And you don’t need to be perfect-just consistent.
Can you have fatty liver without being overweight?
Yes. About 10-20% of people with MASLD are not overweight. This is called "lean MASLD." It’s often linked to insulin resistance, genetics, or poor diet-even if body weight is normal. People with this form may have high triglycerides, type 2 diabetes, or a family history of liver disease.
Is MASLD the same as NAFLD?
MASLD is the new name for what was once called NAFLD. The change happened in June 2023 to reflect that the condition is driven by metabolic dysfunction-not just the absence of alcohol. The new term includes people who have at least one metabolic risk factor, like high blood sugar, high blood pressure, or excess belly fat.
Can MASLD lead to liver cancer?
Yes. If MASLD progresses to MASH and then to cirrhosis, the risk of liver cancer (hepatocellular carcinoma) increases significantly. About 24% of liver transplants in the U.S. are now due to MASLD-related cirrhosis. Early intervention can prevent this progression.
What’s the best diet for reversing fatty liver?
The Mediterranean diet is the most studied and effective. Focus on vegetables, legumes, fish, olive oil, nuts, and whole grains. Avoid added sugar, refined carbs, fried foods, and processed snacks. Studies show 76% of people improve liver fat levels after 6 months on this diet.
How much weight loss is needed to reverse MASLD?
Losing 5-7% of your body weight can reverse simple fatty liver in most people. For those with MASH (inflammation), losing 10% or more can reduce liver inflammation and scarring in about 45% of cases. Even small losses make a big difference.
Are there any medications for MASLD?
As of 2025, resmetirom is the first FDA-approved drug for MASH, the advanced form of MASLD. It helps reduce liver fat and fibrosis. But it’s only for people with moderate to severe disease. There are no approved drugs for early-stage MASLD-lifestyle changes remain the only proven treatment.
Can alcohol make MASLD worse?
Yes. Even small amounts of alcohol can increase liver inflammation and damage in people with MASLD. The American Association for the Study of Liver Diseases recommends complete abstinence. Some European guidelines allow limited intake, but the safest approach is to avoid alcohol entirely.
How often should I get tested for MASLD?
If you have metabolic risk factors-obesity, diabetes, high blood pressure, or high triglycerides-get screened every 1-2 years. A simple blood test for ALT and AST is a good start. If those are elevated or you’re at high risk, ask about a FibroScan. Early detection saves lives.


Ryan Airey
November 15, 2025 AT 14:46This whole MASLD thing is just Big Pharma's way of selling more drugs. They rebranded NAFLD to MASLD so they could patent a new pill. Resmetirom? More like resmehype. If you're telling me the solution is walking and eating vegetables, why the hell is there a $1000/month drug approved? They want you dependent, not healed.
Hollis Hollywood
November 16, 2025 AT 14:19I’ve been living with this for years, quietly, and honestly? The loneliness of it is worse than the disease. No one talks about how exhausting it is to be told you’re ‘just overweight’ when you’ve been eating clean and walking 10k steps for five years. The blood tests come back ‘normal’ but your liver feels like it’s carrying the weight of the world. I didn’t know I had it until my ALT was 120 and my doctor shrugged. That’s not healthcare. That’s negligence wrapped in a white coat. I’m not mad at myself-I’m mad at the system that lets people slip through.
Adam Dille
November 16, 2025 AT 14:41Just started walking after dinner and cutting out soda. Already feel less bloated 😊
Also, swapped my oat milk latte for black coffee-no sugar, no guilt. Small wins, y’all. 🙌
Anyone else notice how much better you sleep when you stop eating sugar after 7pm? I’m obsessed.
Katie Baker
November 17, 2025 AT 10:02I love how this post doesn’t just scare you-it gives you a roadmap. I’m 34, not overweight, but had high triglycerides and a family history. Got my FibroScan last month-score was 8.1. Scared me into action. Started meal prepping Mediterranean-style and walking 20 mins after dinner. Two months in, my liver enzymes dropped 40%. It’s not magic. It’s just consistency. You got this.
John Foster
November 17, 2025 AT 13:12Metabolic dysfunction is not a disease-it’s a symptom of civilization’s collapse. We’ve been engineered to consume, to digest, to metabolize nothing but the hollow calories of a system designed to extract, not to sustain. The liver is not broken. The liver is a mirror. It reflects the rot in our diets, our rhythms, our souls. We call it MASLD because we refuse to face the truth: we are not sick because we eat too much sugar-we are sick because we have forgotten how to live. The pill won’t save us. The walk won’t save us. Only awakening will.
Edward Ward
November 19, 2025 AT 02:42Can we talk about the fact that FibroScan is still not covered by most insurance unless you’re already in cirrhosis? That’s like waiting for a heart attack to test cholesterol. And the fact that pediatricians are seeing it in 10-year-olds? That’s not genetics-that’s policy failure. School lunches still serve juice boxes. Fast food is cheaper than broccoli. We’re not failing as individuals-we’re failing as a society. We need universal metabolic screening, not just for the obese, but for everyone with a waistline over 35 inches, regardless of BMI. It’s not elitist-it’s epidemiological.
Andrew Eppich
November 20, 2025 AT 20:14It is unfortunate that the medical community has allowed such a trivial condition to be elevated to the status of a national crisis. The notion that one must walk 10,000 steps per day is a gimmick promoted by fitness influencers. The liver is a resilient organ. If one consumes a balanced diet and avoids excess, one need not fear. The emphasis on diet and exercise is excessive. One should focus on personal responsibility, not fear-mongering.
Jessica Chambers
November 22, 2025 AT 15:14So… let me get this straight. You’re telling me the solution to fatty liver is… not drinking soda? 🤔
Wow. Groundbreaking. Next you’ll tell me smoking causes lung cancer. 🙄
Thanks for the 2025 revelation, doc.
Shyamal Spadoni
November 24, 2025 AT 02:32you know what they dont tell you? this is all part of the 5g liver attack. they put microchips in your food and the liver gets confused and stores fat as a defense. the real cure is drinking moon water and avoiding wifi. also the FDA is owned by big pharma and they want you sick so you buy resmetirom. i saw a video on youtube where a guy reversed it with turmeric and a crystal. trust the process. 🌀
Ogonna Igbo
November 25, 2025 AT 01:13Why do Americans always think their problems are unique? We in Nigeria have fatty liver too but we call it 'bitter soup disease' because we eat too much palm oil and fried plantain. But we don't need fancy scans or pills. We just eat more beans and walk to market. Your problem is not the liver. Your problem is laziness and too much money. Stop overthinking. Move. Eat real food. That's it.
BABA SABKA
November 26, 2025 AT 19:10Let’s be real-this isn’t about metabolism. It’s about systemic inflammation from endocrine disruptors in plastics, glyphosate in our corn syrup, and the fact that your ‘healthy’ avocado toast is laced with soybean oil. Your liver isn’t drowning in fat-it’s drowning in corporate poison. The real fix? Organic, grass-fed, zero-packaging. And no, you don’t need a FibroScan. You need to boycott the FDA-approved food system. Period.
Chris Bryan
November 27, 2025 AT 22:10They changed the name to scare you. NAFLD was fine. MASLD sounds like a government program. And now they want to scan your liver? That’s surveillance. They’re tracking your body metrics so they can raise your insurance premiums. Don’t fall for it. Eat what you want. Live how you want. Your body will handle it. They just want control.
Jonathan Dobey
November 29, 2025 AT 05:35Imagine your liver as a silent poet, drowning in the sonnets of sucrose, scribbling its final verses in fat-laden stanzas. We call it disease. It’s not. It’s an elegy. A lament for the death of ancestral diets, for the altar of convenience, for the sacred ritual of chewing replaced by swallowing pixels of flavor. The pill? A lyricist’s bandage. The walk? A stanza of redemption. But the real cure? A return to the rhythm of sun and soil, to the silence before the scream of the metabolic machine.
ASHISH TURAN
November 30, 2025 AT 12:05My dad had MASLD. He lost 12% weight with just walking and cutting sugar. No meds. No fancy diets. Just consistency. He’s 72 now, FibroScan normal. If he can do it, anyone can. Start with one change. One day. One meal. That’s all it takes.