Fibromyalgia Symptom Assessment Tool
Fibromyalgia WPI Assessment
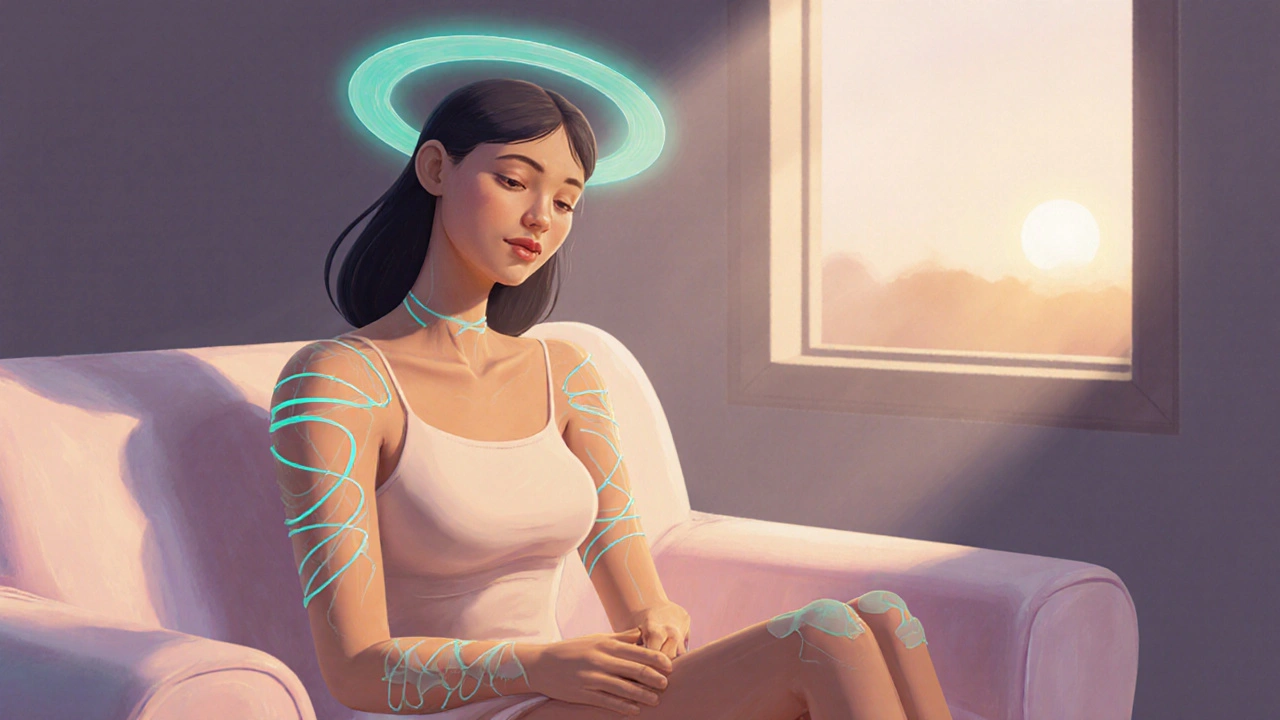
Select all areas where you experience pain (WPI = Widespread Pain Index)
Symptom Severity Assessment
Rate your symptom severity (SS = Symptom Severity Score)
Your Assessment Results
According to the 2016 ACR diagnostic criteria, you need:
- Widespread pain index (WPI) of at least 7 out of 19 body regions
- Symptom severity (SS) score of 5 or more
- Symptoms present for at least three months
Your WPI score: 0 (out of 19)
Your SS score: 0 (out of 12)
Next Steps: If you've had these symptoms for more than 3 months, consider discussing these results with a healthcare provider for a comprehensive evaluation.
This tool is for educational purposes only. It does not replace professional medical diagnosis or treatment.
If you're wondering what fibromyalgia really is, here's the plain‑talk guide that cuts through the medical jargon. We'll walk through what you might feel, why it happens, and what actually helps.
When you first encounter the term, you might picture a vague, "pain everywhere" condition. In reality, Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, fatigue, and a cluster of other symptoms that affect daily life. Researchers estimate that about 2-4% of the population lives with this syndrome, most often women between their 30s and 50s.
What Are the Main Symptoms?
People with fibromyalgia often describe a deep, aching sensation that seems to radiate across the body. The most common signs include:
- Widespread pain lasting at least three months, typically felt on both sides of the body and above and below the waist.
- Tender points: small, localized spots that hurt intensely when pressed (e.g., back of the head, elbows, knees).
- Fatigue that doesn't improve after a full night’s sleep.
- Sleep disturbances such as insomnia, restless leg syndrome, or non‑restorative sleep.
- Cognitive difficulties often called "fibro‑fog," including memory lapses and trouble concentrating.
- Headaches, including migraines and tension‑type headaches.
- Morning stiffness lasting more than 30 minutes.
These symptoms can wax and wane, and many patients report that stress, weather changes, or physical overexertion trigger flare‑ups.
Digging Into the Causes
Fibromyalgia isn’t caused by a single factor. Current research points to a mix of genetic, neurobiological, and environmental contributors.
- Genetics: Family studies show a higher prevalence among first‑degree relatives, suggesting a hereditary component.
- Central Sensitization: The brain and spinal cord become hyper‑responsive to pain signals, amplifying normal sensations into chronic pain.
- Neurotransmitter Imbalance: Low levels of serotonin, norepinephrine, and dopamine can affect pain modulation and mood.
- Stressful Events: Physical trauma, emotional stress, or infections often precede the onset, possibly resetting the nervous system.
- Hormonal Factors: Higher rates in women hint at a role for estrogen and other hormones.
Because the exact trigger varies, clinicians treat fibromyalgia as a syndrome-a collection of interrelated problems rather than a single disease.
How Do Doctors Diagnose It?
There’s no blood test that confirms fibromyalgia, so diagnosis relies on clinical criteria. The most widely used standard is the 2016 revision from the American College of Rheumatology (ACR). It requires:
- Widespread pain index (WPI) of at least 7 out of 19 body regions.
- Symptom severity (SS) score of 5 or more, accounting for fatigue, waking unrefreshed, and cognitive issues.
- Symptoms present for at least three months.
- Exclusion of other conditions that could explain the pain (e.g., rheumatoid arthritis, lupus).
Physicians often combine the ACR checklist with a thorough medical history, physical exam, and sometimes imaging to rule out other diagnoses.

Treatment Options: A Multi‑Layered Approach
No single therapy works for everyone, so the most effective plan blends medication, lifestyle changes, and complementary therapies.
| Category | Examples | Typical Benefits | Potential Risks |
|---|---|---|---|
| Pharmacologic | Pregabalin, Duloxetine, Milnacipran | Reduces pain and improves mood | Drowsiness, weight gain, GI upset |
| Physical Therapy | Low‑impact aerobic exercise, aquatic therapy | Boosts stamina, lessens pain sensitivity | Initial soreness, need for consistency |
| Psychological | Cognitive Behavioral Therapy (CBT), Mindfulness | Improves coping, reduces stress‑related flare‑ups | Requires regular sessions, may be costly |
| Complementary | Acupuncture, Massage, Yoga | Alleviates muscle tension, promotes relaxation | Variable quality of practitioner, limited insurance coverage |
Medication often starts with low‑dose antidepressants like duloxetine, which target both pain and depression. Pregabalin, an anticonvulsant, can calm nerve hyperactivity. Doctors usually prescribe the lowest effective dose and adjust based on side‑effects.
Regular exercise-even short walks or swimming-has the strongest evidence for long‑term symptom reduction. Starting slowly and building up prevents overexertion, which can worsen pain.
Psychotherapy, especially CBT, teaches patients how to reframe pain thoughts, manage stress, and establish healthier sleep habits.
Many patients add complementary methods such as yoga, tai‑chi, or acupuncture. While the scientific backing varies, personal testimonies often note better sleep and lower perceived pain.
Practical Tips for Everyday Living
Living with fibromyalgia is a marathon, not a sprint. Here are real‑world adjustments that can make a noticeable difference:
- Sleep hygiene: Keep a consistent bedtime, darken the room, and avoid screens an hour before sleep.
- Pacing activities: Break tasks into small chunks, rest between them, and use a planner to avoid overdoing it.
- Nutrition: Some sufferers feel better with anti‑inflammatory foods-think omega‑3 rich fish, leafy greens, and berries-while limiting processed sugars and caffeine.
- Stress management: Daily mindfulness meditation (10minutes) can lower cortisol, the stress hormone linked to flare‑ups.
- Support networks: Joining a local or online fibromyalgia support group provides emotional relief and practical hacks.
Remember that setbacks are normal. The goal isn’t to eliminate pain completely but to lower its impact on work, relationships, and hobbies.

Common Myths Debunked
Because fibromyalgia is invisible, misconceptions abound. Let’s clear a few:
- Myth: "It’s all in your head." Fact: Brain imaging shows altered pain processing pathways.
- Myth: "Only women get it." Fact: Men can develop fibromyalgia, though they’re diagnosed less often.
- Myth: "You’ll never improve." Fact: With a tailored plan, many report up to 30% symptom reduction within months.
- Myth: "Exercise makes it worse." Fact: Low‑impact, steady‑state activity actually desensitizes pain pathways when done consistently.
When to Seek Professional Help
If you notice any of these red flags, schedule an appointment promptly:
- Sudden, severe joint swelling or redness (could signal arthritis).
- Unexplained weight loss or fever.
- New neurological symptoms like numbness or weakness.
- Depressive thoughts or suicidal ideation.
A multidisciplinary team-rheumatologist, physical therapist, mental‑health provider-usually offers the best outcomes.
Frequently Asked Questions
Can diet cure fibromyalgia?
There’s no cure through diet alone, but an anti‑inflammatory eating plan can lessen pain spikes and improve energy levels.
Is fibromyalgia hereditary?
Family studies suggest a genetic predisposition, but environmental triggers are usually needed for the syndrome to manifest.
How long does it take to see improvement with exercise?
Most patients notice reduced pain and fatigue after 6-12weeks of regular low‑impact activity, though consistency is key.
Are antidepressants safe for long‑term use?
When monitored by a physician, drugs like duloxetine are considered safe for years, but side‑effects should be reviewed regularly.
What is fibro‑fog and how can I manage it?
Fibro‑fog refers to memory lapses and reduced concentration. Strategies include writing tasks down, using timers, and practicing mindfulness to improve focus.

Malia Rivera
October 17, 2025 AT 13:06America's resolve to tackle any obstacle mirrors the stubborn persistence of chronic pain; we must confront fibromyalgia with the same fierce patriotism we reserve for defending our borders.
When a condition cloaks itself in mystery, it demands a collective, unapologetic stance.
Dismiss the skeptics who claim it’s “all in the head” – the science already proves altered brain pathways.
Our society thrives when we apply the same rigor to invisible illnesses as we do to national security.
Only then can sufferers truly feel the support of a nation that never backs down.
Kate Marr
October 23, 2025 AT 07:59Patriotic spirit fuels perseverance, and that same fire can ignite hope for those battling fibromyalgia 🇺🇸.
Take control of sleep hygiene, move your body, and watch the fog lift gradually 🌟.
Remember, a nation that cares for its people keeps them strong.
James Falcone
October 29, 2025 AT 01:53Yo, if you’re stuck in that endless ache, just start with a short walk, no drama.
Small wins add up, trust me.
Frank Diaz
November 3, 2025 AT 20:46The human condition is a tapestry woven from pain and perception; fibromyalgia is merely a thread that challenges our philosophical comfort zone.
Yet, we must not excuse suffering with lofty rhetoric – action is the true measure of virtue.
When society labels an ailment with skepticism, it reflects a deeper moral failing.
Consequently, we owe the afflicted decisive empathy, not idle debate.
Only then can we transcend the emptiness of hollow patriotism.
Mary Davies
November 9, 2025 AT 15:39In the quiet corridors of our minds, the echo of fibro‑fog drifts like a mournful violin.
It is as if the world conspires to mute our thoughts while demanding we perform.
The drama of daily life becomes a stage where pain steals the spotlight.
Yet, we linger in the shadows, yearning for a script that offers relief.
Valerie Vanderghote
November 15, 2025 AT 10:33Listen, I’m going to lay it out plainly because you deserve every ounce of detail, even if it feels like an invasion of your personal space.
First, the genetics. Yes, your family tree may whisper hints about susceptibility, but that’s just the opening chord of a symphony you didn’t ask to join.
Second, central sensitization – your nervous system turns the volume up to eleven, broadcasting pain like an unwanted radio station that never turns off.
Third, neurotransmitter imbalances; low serotonin and dopamine act like faulty wiring, causing mood swings and making every ache feel like a hammer on your skull.
Fourth, stress triggers – because life loves to throw curveballs, and your body, already on edge, catches them with a painful embrace.
You might wonder how all this translates to daily living, so let’s unpack the practical nightmare.
Imagine waking up, the alarm blares, and your joints scream louder than a construction site, making the simple act of getting out of bed feel like scaling a mountain.
Then you attempt to make coffee, and the fatigue that won’t lift after eight hours of sleep drags you into a fog where thoughts drift like paper boats on a stagnant pond.
Now, add the cognitive fog – memory lapses that make you forget why you entered a room, turning everyday tasks into a bizarre scavenger hunt.
Compounding this, the unpredictable flare‑ups triggered by weather, overexertion, or even a stressful email, turn planning into a gamble.
But there is hope, however faint, in the multilayered approach that clinicians champion.
Medication like duloxetine or pregabalin can temper the storm, though they come with side‑effects that feel like an unwanted guest at the party.
Exercise, the paradoxical hero, tampers the pain pathways if you start with gentle swimming or short walks, gradually building tolerance without shattering your depleted energy reserves.
Psychotherapy, especially CBT, re‑programs the narrative, teaching you to reinterpret pain signals as less threatening, a mental armor of sorts.
Complementary therapies – yoga, tai‑chi, acupuncture – are like soothing lullabies for a restless mind, though their efficacy varies like the wind.
Finally, lifestyle hacks: consistent sleep hygiene, anti‑inflammatory diets, stress reduction through mindfulness; these are the tiny gears that keep the whole machine from grinding to a halt.
In short, fibromyalgia lives in the shadows of biology and experience, but with a coordinated, patient‑centered strategy, you can wrest control back from the chaos.
Michael Dalrymple
November 21, 2025 AT 05:26It is essential to recognize that managing fibromyalgia requires a balanced regimen of physical activity, psychological support, and pharmacologic intervention.
Adopting low‑impact aerobic exercise, such as swimming or brisk walking, has been shown to attenuate pain sensitivity over time.
Simultaneously, engaging in cognitive‑behavioral therapy can empower patients to reframe maladaptive thought patterns.
Together, these evidence‑based strategies constitute a comprehensive approach that fosters both physical and mental resilience.
Emily (Emma) Majerus
November 27, 2025 AT 00:19Start small, stay consistent – thats the key.
Dont forget to log ur progress.
Virginia Dominguez Gonzales
December 2, 2025 AT 19:13Rise above the haze, dear warrior, for each sunrise brings a chance to rewrite your story.
The battle against fibro‑fog may be relentless, but your spirit is an unbreakable flame that refuses to be dimmed.
Embrace the support around you, and let hope be the compass guiding you forward.
Carissa Padilha
December 8, 2025 AT 14:06What they don’t tell you is that the pharma giants have a vested interest in keeping you on a cocktail of meds forever.
Their research boards conveniently highlight side‑effects while downplaying natural remedies.
So when you hear “exercise is the best medicine,” ask yourself who profits from that narrative.
In reality, a holistic lifestyle can outmaneuver any pill, but the system is built to resist change.
The truth hides in plain sight, waiting for those brave enough to question the status quo.
Richard O'Callaghan
December 14, 2025 AT 08:59Look, i gotta be real honest – you cant keep ignoring the signs, its like walkin into a storm without an umbrella and expectin to stay dry.
your body is screaming, and you keep tellin it to hush, that ain't right.
maybe try a talk w a doc, or atleast a physio, stop pretended you got it under control.
Alexis Howard
December 20, 2025 AT 03:53Fibromyalgia treatments are overrated.
Kevin Adams
December 25, 2025 AT 22:46Ah, the saga continues!!!
We stand at the precipice of understanding, yet the abyss yawns with unanswered questions...
Will we ever decipher the cryptic code of chronic pain or remain forever shackled by its relentless whispers???
Only time, and relentless curiosity, will tell.
Katie Henry
December 31, 2025 AT 17:39Dear colleague, while a brief walk may seem modest, it constitutes a commendable initiation into the disciplined regimen requisite for ameliorating fibromyalgia symptoms.
Consistent adherence to such incremental activity, coupled with steadfast resolve, shall undoubtedly engender progressive improvement and fortify overall wellbeing.